by Nutrilicious | Sep 20, 2019 | Thoughts, The Nation’s Health, Education
When it comes to food choices, what should we be advising those suffering from type 2 diabetes to help them manage weight and glucose?
Do we focus on a low carb diet?
Cutting out fat?
Or just the simple principle of sticking to Eatwell guidelines?
Media headlines continue to offer 101 different – conflicting – solutions. So what’s the truth? How can we piece together this apparent mess to best support those with diabetes?
Next week, in the second in our series of diabetes NutriWebinars, expert Dr Duane Mellor, RD, Senior Teaching Fellow at Aston Medical School, Aston University will be exploring these topics.
Looking at how advice has shifted over the past few decades, he’ll be talking through the latest evidence and explaining what health professionals can do to actually help people living with type 2 diabetes.
The webinar will also cover evidence from the last couple of years that shows that type 2 diabetes is not necessarily always a condition for life: through weight loss and maintenance, we can actually help people go into remission.
Fundamentally, it’s about putting the person with the condition at the centre – rather than trying to force them into eating habits that don’t suit their lifestyle, culture or preferences. Instead of concentrating on specific nutrients at specific times of the day – ‘you must have starchy carbs at breakfast’ – it’s working out what works for them, at the same time as creating an overall balanced diet.
Inviting questions and ideas from participants, the NutriWebinar is set to be an interesting, informative and empowering evening. (Plus, it’s free and counts as CPD.) We hope you’ll join us and encourage colleagues to join in too: register now

by Nutrilicious | Aug 19, 2019 | Hot Topics in nutrition, Surveys and insights, Changing mindset
At long last, the Scientific Advisory Committee on Nutrition (SACN) report on saturated fats and health was published this month. The conclusion? Nothing new: saturated fat leads to heart disease and we should limit it to 10% of our calorie intake. So will it finally put an end to the irresponsible advice that abounds suggesting saturated fat isn’t so bad for you?
It’s taken over a year from the draft report to final version because of the number of comments, criticisms and questions as to why certain studies were or weren’t included as part of the overall evidence into sat fats.
The SACN committee has investigated and answered each one, including only the highest quality evidence available. The studies that came to the wrong conclusions about saturated fat were shown to be flawed.
They’re open about certain limitations to the evidence: for example, whether replacing saturated fat intake with carbohydrate can be beneficial. None of the studies look specifically at ‘good’ carbs (for example wholegrain cereals), just at carbs overall. Further research still needs to be done into this.
But the overall conclusion was inescapable: to reduce cardiovascular disease we should lower our intake of saturated fat.
So will high profile influencers like Dr Michael Mosley or Joe Wicks take note and stop promoting ingredients like coconut oil, which is shown to have higher saturated fat than butter and lard?
Sadly, we think it’s unlikely. For one reason or another they seem to have too much invested in it.
But if you’re reading this and feel as strongly as we do about the need to stop the irresponsible advice, join us in canvassing the influencers to open their eyes to the dangers of what they’re suggesting – rather than just thinking about their commercial interests or looking for the next great headline. #saynotosatfat
Go to the British Nutrition Foundation website for a summary of the SACN report findings

by Nutrilicious | Jun 14, 2019 | The Nation’s Health
‘The levy is working.’ That’s the conclusion from a recent survey of drinks sales, a year on since the Soft Drinks Industry Levy (SDIL) – or sugar tax – was introduced.
The study concentrated on products that sell in large enough volume to have a public health effect. In a ‘historic change’, sales of Coke Zero Sugar increased by 50 per cent and Pepsi, sugar-free Max by 17 per cent. Full sugar Classic Coke and Blue Pepsi sales both fell.
The shift is attributed to the sugar free drinks being cheaper than their full sugar equivalent, as a result of the SDIL. Giving consumers the economic incentive to buy drinks that are healthier has worked. As the authors of the study say, ‘Discounts have had the effect that economists expected and health specialists hoped for.’
New sugar free versions of popular drinks are being increasingly sold in major retailers, with the hope that they’ll also become more prominent in smaller, independent shops. The positive trend is moving in the right direction – and it’s happening relatively quickly.
More needs to be done from a retail environment point of view, especially alerting customers to the discounts. Non-lead brands do still have work to do on reducing their sugar levels – although affecting a far smaller number of individuals, they still impact on health. And of course, the drinks industry is just one part of the wider obesity story.
We wondered what the effect of the sugar tax would be when it was introduced. So it’s fantastic to hear the dramatic change that’s already happened – and we’ll be monitoring the year ahead with interest.
The study was carried out by Jack Winkler, Emeritus Professor of Nutrition Policy, London Metropolitan University and Tam Fry, chair National Obesity Forum. Go to BeverageDaily.com to read the full results

by Nutrilicious | Jun 3, 2019 | Hot Topics in nutrition
According to headlines, iodine deficiency is the latest threat to our health in the UK. What’s more, the media says, poor iodine status is due to the rise of veganism and our increasing love for plant-based drinks as milk alternatives.
The headlines focused on the fact that dairy milk is our main source of dietary iodine, whilst plant-based drinks (with a few exceptions) do not contain iodine.
But is lack of iodine an issue? Could an increased consumption of plant-based drinks put people at risk of iodine deficiency?
It’s a complicated issue, but let’s look at the facts…
Is iodine important in the diet?
Yes. Iodine is essential. The body needs iodine to make thyroid hormones, which is fundamental for foetal and young children’s growth and brain development. Severe iodine deficiency in pregnant women can cause irreversible brain damage in their offspring. Population studies have also demonstrated a lower IQ score of around 13 points in severe iodine-deficient populations compared to iodine replete populations. The World Health Organisation (WHO) has stated that low iodine status is the single most preventable cause of brain damage in the world.
Adequate iodine status is especially critical for women of child-bearing age, during pregnancy and whilst breast feeding, to ensure optimal brain development in the foetus and young infant. Continued optimum intake in childhood and adolescence is fundamental as the brain continues to develop. It is important to note that folate, iron and long-chain omega-3 fats are also critical to brain development.
Severe iodine deficiency is rare in developed countries like the UK. However, there are significant numbers of women, especially of child-bearing age who are mild to moderately iodine deficient. A number of recent meta-analysis (including findings from UK population groups) indicate a high probability of compromised cognitive development in children whose mothers had mild to moderate iodine status during pregnancy. How significant these lower IQ scores are to cognitive ability in adulthood has yet to be established.
Measuring iodine status of a population
Median urinary iodine concentrations (UIC) are the best way to assess the iodine status of a population or large group. This is because the iodine content of foods is too variable to rely on dietary intakes as a measure of iodine status.
How the WHO classifies iodine deficiency.
| For a healthy population 6 years and older |
For pregnant and breast feeding women |
| Median UIC is below 100mg/L AND
If 20% or more of that population has a median UIC of less than 50mcg/L. |
Median UIC below 150mcg/L |
| Mild deficiency |
50-99 mcg/L |
| Moderate deficiency |
20-49 mcg/L |
| Severe deficiency |
<20 mcg/L |
Does the UK have an iodine deficiency problem?
According to the latest National Diet and Nutrition Survey (NDNS) using WHO criteria, from an overall population perspective we’re actually not doing badly, with all age groups and sexes showing adequate iodine status.
However, severe to moderate deficiency (UIC <50mcg/L) still afflicts a significant number of our population:
• Approximately 1 in 10 children aged 4-18 years
• 14% of adults 19-64 years
Unfortunately, the NDNS does not currently perform UIC measures in pregnant women or the under 3s, the most susceptible population groups to low iodine status.
Women of child-bearing age (16-49 years) are classified as iodine replete, with a median UIC of 102mcg/L.
However, almost 70% of them would be classified as mildly to moderately iodine deficient if they were to become pregnant – i.e. UIC levels below 150mcg/L – when taking account for the increased demands of the foetus and young infant.
As a result, many are calling for the government to review the UK’s iodine initiatives, especially for women who are planning/are pregnant, or are breast feeding.
How does what we eat impact on our iodine levels?
The ocean is nature’s source of iodine, thus fish, seaweed and algae are rich sources. Additionally, coastal soil regions will acquire some iodine from coastal waters.
Therefore, higher intakes of seafood are paramount for adequate iodine status and studies have found seafood intakes to be positively correlated with iodine status.
In the UK, fish intakes are exceptionally poor. Few meet the government’s recommendation of two 140g servings per week. Average total fish weekly intakes in the UK:
• The majority of 4-18 year olds consume no more than 56g.
• The majority of adult women (19-64 years) consume 84g fish.
• The majority of adult men (19-64 years) consumer nearly 100g fish.
Iodine and dairy milk
In the UK, farming practices were changed in the 1930s to eradicate the high incidence of iodine deficiency. Animal feeds were fortified with iodine and the use of sterilizers containing iodine were introduced. This resulted in a significant increase in iodine levels of dairy milk and a consequent eradication of severe iodine deficiency.
Winter milk is significantly higher in iodine compared to summer milk, as dairy cattle are more likely to reared indoors with fortified feed in the winter months.
Thus the key source of iodine in the UK is indeed dairy milk – contributing to 34-40% iodine intakes in adults and 40-51% iodine intakes in 4-18 year olds.
Could plant-based drinks place the nation at risk of Iodine deficiency?
It is true that the majority of plant-based drinks do not contain iodine. However:
1. Incidence of mild to moderate iodine deficiency in pregnant women has actually been high in the UK since the 1990s, when milk intake was at its highest.
2. Despite the recent popularity of plant-based drinks, dairy milk intakes have seen little reduction. And plant-based drinks consumers also continue to drink dairy.
Since 2010, milk intakes have reduced by just 74mls per person per day (a 6.5% decrease), while plant-based drinks – although on a sharp incline – equate to just 45ml per person per day.
Therefore, plant-based drinks – whether they are or not fortified with iodine – are not the cause of the iodine deficiency that has been present for many decades.
Other considerations
• Cognition is affected by multiple environmental, psychological as well as dietary components e.g. pollutants, home environment, education level, various nutrients including vitamin D, iron, folate and iodine.
• Iodine is not highlighted in advice provided to expectant mothers, nor is it on the government agenda.
• No studies have indicated vegan populations, who exclude all dairy, to have lower IQ levels compared to omnivores.
There are also effective initiatives that have helped to eradicate severe iodine deficiency
• The WHO Iodized Salt programme has been adopted in many countries and proven to be successful.
• Iodine supplements have shown to be effective when given to women in the first or second trimester of pregnancy.
Takeaway messages
1. Many factors are at play when considering brain development of the foetus and young infant:
– Adequate intake of a number of nutrients, including iodine but also iron and folate
– Optimal environmental and psychological settings.
‘Fixing’ one aspect or one nutrient is not the answer to helping optimise cognition in the UK.
Saying this, iodine is one of the essential nutrients for brain development. That has been overlooked and needs to be addressed by the government, on a similar level to iron, folate and vitamin D – especially for expectant women and breast-feeding mothers. Monitoring iodine status needs to be instigated by the government for these groups and young children.
2. The increase in plant-based drinks’ popularity is not the cause of the sub-optimal iodine status in the UK, which has been prevalent in pregnant women for decades – way before plant-based drinks became mainstream.
Rather, the poor dietary patterns of the UK population need to be addressed, especially with regard to our less than optimal fish intake – the richest source of iodine.
Whenever we see the media headlines expounding the ‘benefits’ or ‘dangers’ of individual nutrients or foods, we worry. After 20 plus years in public health nutrition and communications, we believe there is a responsibility and an urgent need for all involved in this field to move away from doing this. In the majority of cases it’s not helpful and is more often scaremongering.
a. We need communications to focus on a balanced food intake. Focusing on a single nutrients in the media is dangerous and ignores all the bigger questions that need addressing: especially obesity and its many associated diseases and “how to” best help the nation enjoy a healthy balanced food intake for optimum health.
b. We need food and health communications that are not only healthy but also sustainable for our planet. Current scientific evidence repeatedly highlights the impact that our food choices have on the environment because of their significant contribution to greenhouse gas emissions, deforestation, biodiversity loss, and destruction of the ecosystem, use of fresh water and polluting of soil.
Beef and dairy cattle farming have been highlighted as the major dietary contributors, whereas plant-based drinks have been shown to be significantly more sustainable.
Leading experts have concurred that a balanced diet that is based predominantly on plant foods – including plant-based drinks – with lower intakes of meat and dairy, without having to exclude them altogether, is both sustainable and nutritious. Read our Sustainable Diets blog for more information.
It is incumbent upon all food and health influencers to incorporate these messages into all relevant food and health communications. Unfortunately, this is not yet being considered widely.
Sources:
1. Chambers L. Are plant-based milk alternatives putting people at risk of low iodine intake? Nutr Bulletin 2018;43:46-52
2. PHE. Results of the National Diet and Nutrition Survey (NDNS) rolling programme for 2014 to 2015 and 2015 to 2016. 2018 [cited 5/11/2018]
3. WHO-UNICEF. Assessment of iodine deficiency disorders and monitoring their elimination. Third Edition. 2008 [cited 9/25/2018]
4. Bath S, Rayman M. A review of the iodine status of UK pregnant women and its implications for the offspring. Environ Geochem Health 2015;37(4):619-29.
5. Levie D, Korevaar TIM, Bath SC et al. Association of maternal iodine status with child IQ: a meta-analysis of individual-participant data. J Clin Endocrinol Metab. 2019 Mar 28. [Epub ahead of print]
6. Dineva M, Rayman MP, Levie D et al. Similarities and differences of dietary and other determinants of iodine status in pregnant women from three European birth cohorts. Eur J Nutr. 2019 Feb 8. [Epub ahead of print]

by Tanya HAFFNER | May 15, 2019 | Retail, Hot Topics in nutrition, Thoughts
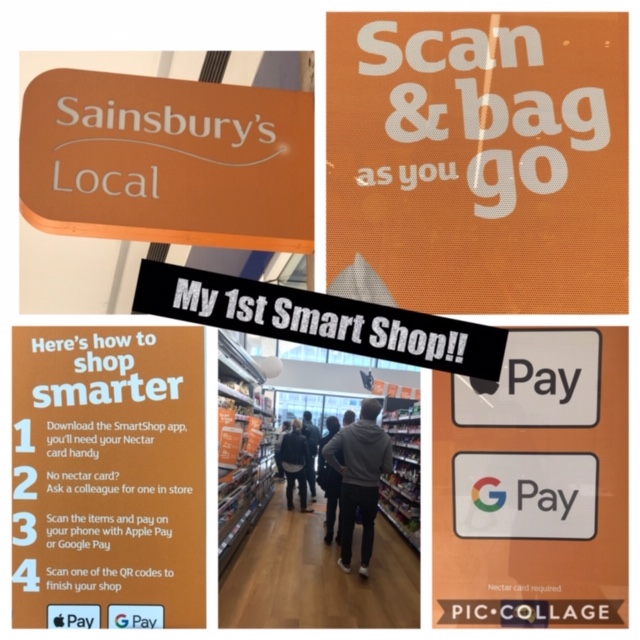
My first SMART SHOP 🛒 ever!
A taste of the future of grocery shopping! 🍏 🍊 🥛
Have you experienced it yet? If so how was it? This is my short story….May 2019!
“I can do this”…I told myself as I hear my forever forward thinking colleague Howard @see_research tell me that @Sainsburys @SainsburysNews have a new smart shop in Holborn – must be tried!
Forget ones inbuilt fear about new tasks I tell myself, especially new tech tasks….which is always a slow learn for me, where I normally have to do things 2-3 times before it clicks! Instead, need to muster all life skills accumulated over many years to overcome said fear, gain new experience, stay ahead & be more informed about retail advances!
Swapping 👠 for 👟 after our meeting I bounce over to the new store with curiosity & best enthusiasm possible for joining in…thankfully greeted by helpful friendly young millennial providing immediate, necessary, app set up assistance & source of calm!
After 10 mins setting up the store app on my 📱 (not as easy as I had hoped with millennial help but thankfully unlike the much slower paced android next to me 😢 ) I was finally ready to go & shop like I never shopped before & looking forward to experiencing no checkout & a speedy exit!
I watched & copied those before me! I test scanned an 🍏 . I scanned the bar code on the apple shelf, then picked up the apple & placed it in my bag. Easy! “Whoopee” I say when camera scans it immediately. I briefly remind myself of a talk at my sons school the week before which inspired me to embrace tech +++ + as our near future is artificial intelligence in every which way possible. Suddenly feeling more positive about my chances with that! What fun! 😀
Onto the next shelf I tried to scan the bar code on the shelf in front of a pack of mixed fresh beans. Error appears! 😆Oh dear. You have to fail before you really succeed, right?! I discover that for packaged goods you have to scan the bar code on the pack – not the shelf! A little awkward & challenging when holding the product & my shopping bag & in need of at least one whole hand to take the scan on the iPhone & another hand to hold the product. But must not be defeated!
I scan two more items successfully. I then suddenly think about my next meeting & the need to run. I smugly look at the long queue in front of me & start to proceed to check out & pay on the spot on my app & search for the QR code on the shop wall to indicate Im done & leaving. Only snag….my apple pay linked to the app doesn’t accept @Barclays @BarclaysUK debit cards yet ,which explains the difficulties that even my helpful millennial did not realise at set up!
A bit frustrating having to leave & not complete the new task- but having no time for the store queue the store manger kindly takes my items back.
I did however leave thankful to @Sainsburys overall for the new shopping experience. It was of course a faff to set up the app even for the millennial assisting me and it obviously has a teething problem with some banking cards. However, once set up & you know where to scan I can only imagine it becoming second nature to us all very quickly.
On the negative side I can see us having no human contact as we go out to shop which adds to my concerns about the deterioration in social skills as tech inevitably increases in our lives. A big responsibility for the big tech corporations & us all to address, I think.
On the positive side I can visualise all kinds of new nutrition tech supporting this app that may analyse our shop as we scan, potentially feedback to us as we shop & help nudge us towards healthier & more sustainable shopping baskets! How amazing would that be!
Watch this space… I have no doubt! If you have experienced smart shop or have any further thoughts Id love to hear! In the meantime happy 😃 healthy shopping everyone however you choose to do it right now! 🛒

by Nutrilicious | Apr 16, 2019 | The Nation’s Health, Changing mindset, Impactful health initiatives
We’re excited to be involved in a new initiative to help tackle the critical problem of poor diet amongst lower income households: Shop Well – Eat Well. It’s a collaboration between the British Dietetic Association (BDA), Alpro and the Southwark Hub, with the aim of a multi-angled approach to have a real and lasting impact.
Launched last month, we brought together experts to give their insights into key topics. Here’s a summary of some of the key points, followed by links to each of the presentations, which we highly recommend you take the time to watch!
People on lower incomes have a worse diet and shorter life expectancy
There is a direct correlation between diet and income, in turn affecting health. The lower your income, the more likely it is you will:
- Eat more sugar, processed foods, fat and sodium
- Eat less fibre, vitamin A and folate
- Be less likely to meet iron, folate and calcium recommendations
- Eat less oil-rich fish
- Eat more take-aways
- Cook less at home from scratch
People in lower income groups in the UK have a significantly shorter life expectancy than the average: by nine years for women and seven for men.
They have double the rates of cardiovascular disease, lifestyle-related cancers, type 2 diabetes and total mortality compared to the national average. Obesity prevalence of the most deprived 10% of children is approximately twice that of the least deprived 10%.
This is not new news. Countless attempts have been made to try to address the problem and encourage people on lower incomes to eat more healthily, thereby increasing their quality of life and life expectancy.
But when it comes to eating habits, behaviour change is very difficult to achieve.
Barriers to healthy eating are multiple, complex and interlinked – psychological, financial, environmental, conscious and unconscious. Among lower income households they include:
- Financial barriers – For low income families, a big barrier to buying new foods or going to a new food shop is not knowing how much the food will cost, or assuming that it will all be expensive. Parents want to know exactly how much their shopping basket is before they reach the checkout.
- Social barriers – Food habits get passed down the generations as young people grow up and become parents themselves. What children see their parents and families doing is what they grow up thinking of as ‘normal’.
- Preparation space – Cooking from scratch relies on kitchen equipment, confidence in cooking skills, time to prepare food and pleasant surroundings – not the case for many on low income.
- Limited bandwidth – The cognitive burden of living under financial strain and other modern day life stresses reduce parents‘ mental bandwidth; brainpower that would otherwise go to planning ahead and problem-solving.[1] Families in this situation look for quick and easy ways to eat, and takeaway and convenience foods provide an in-the-moment solution to feeding children quickly, affordably and safely.
- Advertising and shop layouts – Cues such as special offers, advertising for takeaways, attractive packaging and child-height shelving nudge families towards less healthy foods in shops.
- It’s not always a lack of knowledge or cost that’s a problem, it’s translating knowledge to practice.
In fact, most eating behaviour is driven by unconscious, habitual processes. These are largely immune to education when it comes to behaviour change. Yet this has been our predominant approach to changing dietary behaviour!
Breaking the habits of a lifetime
Multiple collaborative strategies are needed to succeed in changing behaviour: from government, local authority, industry and all food providers, alongside continuing to help individuals overcome their personal barriers.
We need to making healthy eating
- easy,
- habitual, and
- normal
As behavioural psychologist Dr. Paul Chadwick says, it’s not sustainable for people to have to think about every food choice that they make. Healthy eating has to become the default option.
A new initiative for change
Behavioural science shows the importance of interactions between the individual and their physical and social environment when it comes to habit forming and breaking.
It’s time the food environment changed to make healthy eating as easy to attain as possible for all, including low affluent groups.
It’s also time for families and individuals to be supported in overcoming barriers to breaking the unhealthy habits.
 We’re excited to be part of the new initiative, Shop Well – Eat Well, to help enable this – especially targeting those on a low income.
We’re excited to be part of the new initiative, Shop Well – Eat Well, to help enable this – especially targeting those on a low income.
Starting as a year-long pilot in Southwark, South London, it’s kicking off in June. Community charities and volunteers will join to create peer and professional-led healthy eating seminars and workshops tailored to the young, old and families.
At the launch, Kate Arthur, UK External Scientific Affairs & Nutrition Manager at Alpro, explained: “We wanted to find interventions that would encourage people to think about their food choices differently.
“Going directly into the community to find out what will work for people is the logical thing to do. We’ll be working on different engaging activities such peer led cookery workshops and drop in seminars, with help from the BDA Let’s get Cooking and an advisory committee of experts, always with an eye on the main barriers.
“Ultimately, we’ll be assessing to see what really makes a difference over the next year of the campaign and we’ll share any success stories widely with local communities nationwide and the dietetic community as a whole.”
Caroline Bovey, Chair of the British Dietetic Association added: “By partnering on this project, and working with the food manufacturers and shops that people are accessing daily, we’re excited to directly tackle some of the wider barriers to healthy habits in a local area. The BDA is delighted to be working with Alpro and the Southwark wellbeing hub to help people who often have to prioritise the other demands of daily life over their food choices.”
Take advantage of insightful presentations and useful resources
At our launch, five leading experts presented the latest evidence and initiatives to help overcome barriers to healthy shopping baskets and healthy eating. The presentations are available on the Shop Well – Eat Well website. Make yourself a cup of tea, watch, learn and be inspired:
– Dr Paul Chadwick, behaviour change leading expert: A scientific approach to behaviour change
– Sue Baic, Registered Dietitian: Affordable, healthy and sustainable eating in practice
– Duncan Brown, Development Director at charity Shift design: How does affluence impact on food choices?
– Kate Arthur, Alpro UK’s External Scientific Affairs & Nutrition Manager: Changing behaviour in the community
– Nilani Sritharan, Company Nutritionist at Sainsbury’s Supermarkets Ltd: Making healthy shopping easier
You’ll also find practical and engaging resources to help consumers overcome their barriers to healthy eating.
#shopwelleatwell @SouthwarkHub @BDA_Dietitians @Alpro