by Nutrilicious | Apr 25, 2016 | Food category comment
The growing trend for breakfasting on-the-go and at out of home establishments has been threatening breakfast cereal’s number one spot1. As well as a need for more convenience, breakfast cereals have been hit hard by the recent negative headlines with regard to their sugar content. But are the latest trends going to help improve or will they fuel the obesity epidemic?
What do the Brits fancy for breakfast?
Many surveys claim that up to 42% of us (and almost a quarter of school children) do not always have breakfast, stating time constraints are a major factor2,3. Kantar’s data however shows that only 7.7% of breakfast occasions were actually missed last year. This significant difference could be explained by the growing trend of eating ‘on-the-go’ or away from home which has grown by 10%4.
The UK seems to be slow to change its breakfast habits with the majority of breakfast occasions (84%) still taking place at home and breakfast cereals, toast and porridge remaining top favourites during the week whilst cooked breakfast continues to be popular at weekends2. The growing trend is for eating at catering establishments and portable on-the-go offerings with perceived health credentials such as breakfast biscuits, porridge pots and fruit and nut category, the latter seeing a 21.5% increase in 20152.
Breakfast cereals: UK’s no.1 choice with wholegrain cereals chosen by 37% of us during the week and still claiming over half the share of the market5,6. Many breakfast cereals have now significantly reduced their sugar levels, more ‘no-added-sugar’ variants are gaining shelf-space whilst a few indulgent variants still remain. According the to the latest National Diet and Nutrition Survey (NDNS), breakfast cereals account for just 5% of the added sugar intakes of adults and 6-8% of 4-10 year olds and teens.7 On the other hand, breakfast cereals (especially those that are fortified) do make a significant contribution to key vitamin and mineral intakes:
- B vitamins, in particular B1, B6 and folate.
6-9% of our vitamin D intake – vitamin D status is a growing concern in the UK6.
- Iron: 46% of teenage girls, and almost a quarter of women consume below the low reference nutrient intake (LRNI), which places them at high risk of deficiency. Cereals are a major source of iron contributing to 17% of teens, 23% of 4-10 year olds and 12% of adult intakes.
- Calcium: mainly due to the addition of milk but a handful are also fortified. Almost a fifth of teenage girls do not meet their LRNI placing them at higher osteoporosis risk in later life.
Looks like a hard act to follow, so how do other breakfast choices match up?
Porridge: Oats are making a come-back with 27% of us likely to make this choice in a week5. Porridge oats get a nutritional gold star from us, as they provide the gel-like fibre, beta-glucan, which has been proven to lower cholesterol levels – and boy almost 60% of us need to lower our cholesterol.8,9 However, how we serve them up is critical – piling on the sugar (even demerara sugar), drizzling with honey or syrup and making it with full cream milk converts this saint to a sinner. The porridge revival could be partly explained by the growing ‘on-the-go’ varieties which are now purchased by 9% of consumers4.
Toast continues to be popular for 32% of people during the week5. White toast provides calcium (accounting for 13% of teenagers’ intakes) whilst wholemeal and seeded breads provide fibre which, is highly relevant considering the 2015 new increased UK fibre recommendations6,10. Clearly, what we add to our toast is central to the nutritional quality, nut butters and unsaturated fat spreads providing healthy heart fats, whilst chocolate spreads (yes…that includes the favourite hazelnut and chocolate spread) and preserves are taking us on a sugar high.
Eggs: we can’t seem to get enough of them. Almost 3,000 million eggs are eaten at breakfast every year with one in five of us opting for an eggy breakfast at least once a week11. Eggs, originally classified as a complete nutrient food, provide protein, vitamin D, iron, phosphorus, iodine and selenium. In addition, it is reassuring to know that all the UK heart and health advisory bodies do not limit egg consumption (as the cholesterol found in food does not have a significant effect on blood cholesterol in most people)12. A gold star from us, if boiled or poached, however, the Brits favourite is a fried egg… oops, too much fat.
The growing convenience breakfast trends
Convenience, portability and time-saving options which also provide exceptional nutrition credentials are now in demand. A third of us are eating breakfast away of home at least once a week and 15% of us do so every day according to a Beacon 2015 survey13. In addition, gluten-free and high-protein health claims are also gaining traction4.
Out of home establishments:
- Greggs and MacDonald’s have a booming breakfast trade, however, the majority of options seem to include sausages and / or cheese which is a recipe for a heart attack with the hefty dose of saturated fat and salt levels. Some of the breakfast options providing up to 80% of daily saturated fat and over ¾ of daily salt recommendations. On the positive note, porridge oats are making an entry, however, for consumers to pick out the handful of healthier options amongst the sea of unhealthy options will be difficult. We feel a better balance and better promotion of healthier options are needed.
- Coffee shops: Coffees and other drinks on offer can be high in saturated fat and sugar laden, however, the options are there to opt for lower fat milks and sugar-free syrups. The mainstream coffee shops have improved their ‘healthier’ breakfast options with porridge, fruit salads, fruit and nuts and yogurt with granola on offer. However, the low fibre, higher fat and calorie croissants and muffins continue to be more popular.
- Cooked breakfasts: This is still a popular weekend choice, but with a whopping 800-1,000 calories for a classic fry-up, it has to have a thumbs down from us. Or does it? Making a few requests when ordering can bring this fat and calorie laden classic into healthy repute: poached eggs, beans, grilled lean bacon rasher, mushrooms, tomatoes, one sausage and toast instead of fried bread could almost half the calories whilst still providing fibre, protein as well as essential vitamins and minerals.
On-the-go options
Breakfast drinks, breakfast biscuits and fruit and nut bars have become widely available, albeit at a higher unit cost. All are portion controlled, the breakfast drinks use skimmed milk as the main ingredient and most provide a range of vitamins and minerals – many matching the nutrition profile of breakfast cereals.
Breakfast biscuits: 19% of consumers are opting for breakfast biscuits over cereal bars4. Nutritionally, they mimic cereals from macro and most micronutrients. Calcium and protein levels from the milk added to cereal are clearly lacking in the biscuits, but the leading brand provides clear advice on paring up the biscuits with yogurt and / or fresh fruit / fruit juice. An excellent option in our point of view.
Breakfast drinks: Definitely a very small but growing market that has failed to take off in the past. The Australian number one brand is definitely leading on this category. Many utilise key health slogans such as protein, energy and fibre whilst omitting to highlight their less than impressively sugar content. Nutritionally, they seem to match up with for fat and protein, however, sugar content varies between 18g and 20g per serving compared to cereal at 0-11g per serving. Interestingly, protein content can be exceptionally high and calcium levels per serving are 2 – 3½ fold greater than for most cereals served with milk. This may be advantageous if it appeals to the 19% of teenage girls and 12% of young women who have calcium intakes below the low reference nutrient intakes. Nutrilicious opinion: get that sugar down.
New opportunities
Recent government advice has highlighted the need to cut sugar levels (free sugars to less than 5% total energy intake) and increase fibre intake (to 30g AOAC per day for teens and adults)10. Considering this advice it would seem beneficial for any new breakfast foods to be based on wholegrains and / or provide soluble fibres such as beta-glucans and inulin and to be limited in free sugars as much as possible. The vitamin and mineral fortification of breakfast cereals significantly contributes to the nation’s micronutrient status, thus any new options must ensure that these essential nutrients are not lacking<sup>6</sup>. With on-the-go eating and eating at out of home establishments becoming more popular, it is paramount that options lower in sugar dominate. Sugar is now the big enemy under scrutiny by government, health organisations and pressure groups such as Action on Sugar14. This also applies to porridge pots and cereal pots as not all are low sugar and/or high in fibre. To add to the challenges for innovation, the consumer continuous to demand a great taste as well as a healthy nutrition quality.
Conclusion
When comparing different options, it is clear that healthier options are available whether breakfasting at home, catering establishment, coffee shop or eating on the go. However, the new trends need to focus more on providing a better balance and promoting more of the healthier options. The porridge, fruit and nut, lower fat and sugar free options at catering establishments are a good start, but the likelihood of the consumer choosing these amongst the overwhelming selection of higher fat, salt and sugar options is questionable. Breakfast cereals do contribute significantly to vitamin and mineral intakes especially iron and calcium – and there is a risk for vulnerable groups to become deficient if they begin to move away from these.
With all the above in mind, there are many opportunities to develop new innovative ways to create tasty, convenient, nutritious breakfasts that allow for people on the go to eat a greater variety of foods to help meet their nutritional requirements. Whilst time may be limited for many in the morning, Variety is King in helping consumers achieve adequate nutrient intake.
References
- Financial Times Oct 3 (2014). Daneshkhu S: Cereal sales go soggy as breakfast shrinks. http://www.ft.com/cms/s/0/771a89b2-4af2-11e4-839a-00144feab7de.html#axzz3zVYhDqes
- Agriculture and Horticulture Development Board (AHDB) for Cereals & Oilseeds Market News: Cereals and bread still breakfast mainstays. 14 January 2016. http://cereals.ahdb.org.uk/markets/market-news/2016/january/14/prospects-cereals-and-bread-still-breakfast-mainstays.aspx
- British Nutrition Foundation. National Pupil and Teacher Survey 2015 UK Survey Results. https://www.nutrition.org.uk/attachments/article/846/UK%20Pupil%20and%20Teacher%20Survey%20Results%202015.pdf
- Grocer March Guide to Breakfast.
- Shake Up Your Wake Up, Fun Breakfast Facts (2015). http://www.shakeupyourwakeup.com/why-is-breakfast-important/our-breakfast-foods/fun-breakfast-facts
- Bates B et al (2014). National Diet and Nutrition Survey: results from Years 1 to 4 (combined) of the rolling programme for 2008 and 2009 to 2011 and 2012. Available at https://www.gov.uk/government/statistics/national-diet-and-nutrition-survey-results-from-years-1-to-4-combined-of-the-rolling-programme-for-2008-and-2009-to-2011-and-2012
- Scientific Advisory Committee on Nutrition 2015. Draft Vitamin D and Health report. Scientific consultation: 22 July to 23 September 2015. Available at https://www.gov.uk/government/consultations/consultation-on-draft-sacn-vitamin-d-and-health-report
- Heart UK (2016). The Power of Oat Beta Glucan. http://heartuk.org.uk/images/uploads/healthylivingpdfs/HUK_factsheet_F09_OatBetaGlucanF.pdf
- Townsend N, Bhatnagar P, Wilkins E, Wickramasinghe K, Rayner M (2015). Cardiovascular disease statistics, 2015. British Heart Foundation: London. Available at https://www.bhf.org.uk/publications/statistics/cvd-stats-2015
- Scientific Advisory Committee on Nutrition (2015). Carbohydrates and Health Report. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/445503/SACN_Carbohydrates_and_Health.pdf
- Egg Info (2016). Industry Data. https://www.egginfo.co.uk/egg-facts-and-figures/industry-information/data
- Gray J and Griffin B (2009). Eggs and dietary cholesterol – dispelling the myth. Nutr Bull 36,199-211
- Beacon. Brits’ breakfast habits a big boost for the economy as people spend £76 million every day on eating out for breakfast. Survey 2015. Available at http://www.digitalnewsroom.co.uk/beacon/brits-breakfast-habits-a-big-boost-for-the-economy/
- Action on Sugar (2015). Breakfast Cereals Survey 2015. http://www.actiononsalt.org.uk/actiononsugar/Press%20Release%20/146900.pdf

by Nutrilicious | Mar 21, 2016 | Hot Topics in nutrition
Wednesday 15th March saw the nation’s health top of the government agenda with the launch of the new Eatwell Guide and more surprising, the new budget announcement declaring a tax for sweetened beverages.
We are still in the dark about the how much tax will be added, but it is thought that it will be set at the PHE recommendation of 20%, despite the National Obesity Forum recommendation to set it at 50% if any impact on behaviour change is to occur.
Which soft drinks will be hit?
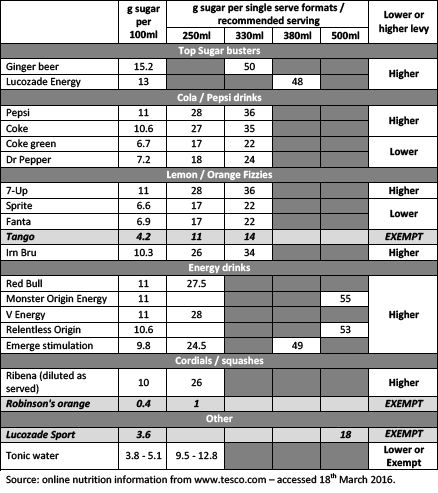
Two tax levels will be set. One for soft drinks providing more than 5g sugar per 100ml and a higher levy for those providing more than 8g sugar per 100ml. The table below indicates how the current soft drinks market will be taxed.
Nutrilicious feels that single serve formats should have been taken into consideration when setting the sugar benchmarks, similarly to front of pack traffic light labelling. As an example, sports drinks are only available as a single 500ml serve bottle providing a total of 18g sugars, yet because they contain less than 5g sugar per 100ml, they will be exempt. This could be argued by other soft drinks companies as unfair. Many that will be taxed for containing over 5g or 8g sugar per 100ml, offer much small single serve formats, limiting the total serve sugar intake to the same as sports drinks and sometimes less.
Exemptions: fruit juice, milk drinks and small producers. This does muddy the waters somewhat as the government in its new sugars recommendations classified fruit juice as a ‘free sugars’ source and why are small producers exempt if they do produce high sugar drinks? Not quite an even playing field and this will not encourage innovation for lower sugar products from companies who will be exempt. Also, what does ‘milk drinks’ refer to? Will sugar laden flavoured milk drinks be exempt?
When will it be enforced? The tax will come into force in April 2018, giving manufacturers adequate time to reformulate their drinks and / or change their offerings to consumers. Many could try to reduce their sugars from the higher to the lower levy benchmark.
Will this reduce consumer purchase of higher sugar soft drinks? Possibly not, but the government is banking on this levy to add over £500 million to the economy which will be used to:
- Double the primary school PE and sport premium.
- Give 25% of secondary schools increased opportunity to extend their school day to offer a wider range of activities for pupils, including more sport.
- Expand breakfast clubs in up to 1,600 schools.
So, Jamie has won the battle to place taxes on sweetened drinks and this will be welcomed by health organisations even though many of them wanted to see a significantly higher levy. We do feel that a more even playing field should have been set and all high sugar drinks, including fruit juice and drinks from small producers, should have the levy enforced. In addition, single serve formats should be considered when assessing sugar levels. If anything, this could go a long way to help prevent consumers’ from being misled by marketing claims that a soft drink ‘is full of / provides energy’. A clever abuse by some manufacturers regarding consumer’s misunderstanding of the word ‘energy’ relating to healthiness rather than empty unnecessary calories. We look forward to more specific details.
A selection of current soft drinks on the market, their sugar content per 100ml and their single serve format or recommended serving size and which tax level they will incur in April 2018.

Sugar Drinks details
For further information on the 2016 budget: www.gov.uk/government/publications/budget-2016-documents/budget-2016

by Nutrilicious | Mar 18, 2016 | Hot Topics in nutrition
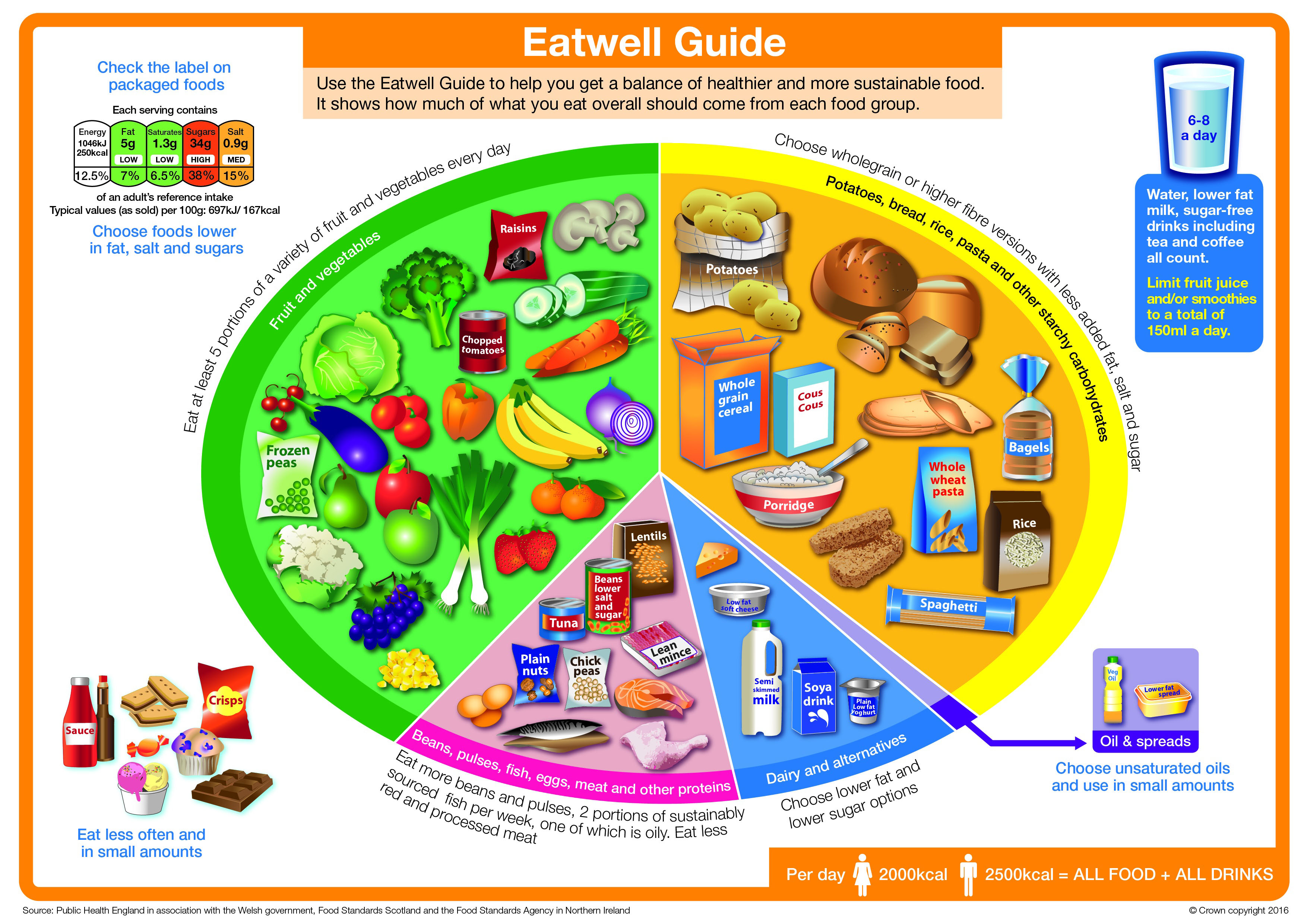
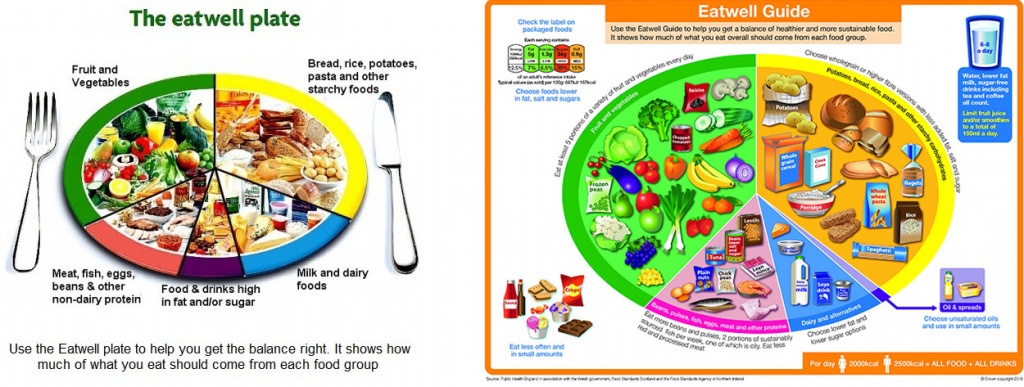
Kept under much secrecy, the government revealed the updated Eatwell Plate to the nation on Thursday 17th March following a stakeholder meeting on Wednesday 16th , which we were pleased to attend. Surprising for us, the changes to the new Eatwell Guide went beyond some simple cosmetic adaptations. In the main, the plate, based on exhaustive reviews of the scientific evidence, has embraced more of the 21st Century consumer eating trends and the growing concerns around sustainability. Will it be more effective at improving the population’s poor nutritional status and reduce obesity? As with all dietary guidelines, effective communication and behaviour change strategies that follow will be key.

Can you spot the 13 differences?
The official documentation lists 12 differences, however, we’ve added one more!
- Importance of hydration has finally been embraced! With recommendations to consumer 6-8 glasses of fluid daily: water, sugar free drinks including tea and coffee and milk.
- Front of pack labelling: possibly coming to terms that as much as we would love the nation to be keen cooks, ready meals and take-aways are by far more popular.
- High fat, salt and sugar foods removed altogether: ‘no role in a healthy balanced diet.’ At last, the group that also included healthy unsaturated fat oils and spreads has been better clarified with latter remaining within the Eatwell Guide as a much smaller section (taking up just 1%).
- Calories have been included for adult men and women – to remind consumers that all foods contribute to calories.
- Four of the five food segments renamed: changing the emphasis to embrace more wholegrains and plant foods whilst keeping saturated fat down.
• Bread, rice, potatoes pasta and other starchy foods is now ‘Potatoes, bread, rice, pasta and other starchy carbohydrates’ with an overarching sub-line ‘Choose wholegrain or higher fibre versions with less added fat, salt and sugar.’
• Milk & dairy foods is now ‘Dairy & alternatives’ with the sub-line ‘Choose lower fat and lower sugar options.’
• Meat, fish, eggs, beans and other non-dairy sources of protein is now ‘Beans, pulses, fish, eggs, meat and other proteins’ with the sub-line ‘Eat more beans and pulses, 2 portions of sustainably sourced fish per week, one of which is oily. Eat less red and processed meat.’
• Food and drinks high in fat, sugar and/or salt has now been removed and instead replaced with ‘Oil & spreads’.
- The five food segments re-sized:
• Fruit and vegetables – go up by 7%, now making up 40% of the plate.
• A bigger push for wholegrain carbs – and up by 5% to 38% of the plate. We hope this will help towards the fight against the ‘anti-carb-based on dodgy and misinterpreted science’ brigade. – As well as wholegrain, there is more emphasis (we feel within the full guidance notes) that it’s not carbs that are fattening but what we choose to add to them.
• Dairy and alternatives – almost halving the recommendations from 15% down to just 8% of the plate. We are pleased to see calcium fortified and unsweetened dairy alternatives making a bigger noise here. And interestingly, 1% dairy milks are recommended over semi-skimmed.
• Protein segment making up the same proportion as previously, has significantly been revamped to embrace sustainability and the need for more plant-based protein consumption. With ‘other proteins’ including soya and Mycoproteins. Single portions of meat to be 70g and fish to be sustainably sourced.
- Fruit juice removed from the Eatwell Guide fruit and vegetable visual in this sector, but highlighted in the hydration section with a significant emphasis that no more than 150ml daily consumption.
- Smoothies have lost their halo: previously, smoothies were permitted to count as 2 of our 5-a-day at 125ml per portion. With both smoothies and fruit juice now classified as ‘free sugars’ the consumption of either has been clearly limited to no more than 150ml per day as part of hydration and contributing to just one of our 5-a-day.
- Oils and spreads: now making just 1% of the Eatwell Guide and thankfully no longer considered as part of the high fat, salt and sugar foods. There is good emphasis within the guidance that all fats however add cals and should be limited.
- Additional messages for further guidance – helping consumers better understand the visuals including 8 tips for healthy eating.
Some changes based on qualitative stakeholder and consumer insights, but considered more cosmetic by us:
- No fork and knife
- Change of name from Eatwell Plate to Eatwell Guide
• Both the above changes based on insights that they little reflect how consumers see meals / consume foods.
- Drawn food images rather than photography. Interesting insight that although stakeholders prefer the latter, consumers prefer the former.
Great strides – but will it be enough?
We are disappointed that there continues to be no offer of practical and household portion guides particularly for the carbohydrate and some foods from the protein groups. This will make it difficult for both the consumers and health advisors to provide the real practical much needed approach. We appreciate that it is a challenging task but believe it to be achievable. As Dietitian communicators in public health we are aware of how much the public needs to be shown how to put these guidelines into practice and how much a consistent approach is needed. PHE at the stakeholder meeting mentioned that they have done some preliminary work on this internally but such things like meal plans will not currently feature in the tools and communications, due largely to lack of funding. We were also surprised that no quantitative survey work representative of the population and health advisers using the tool had not been undertaken prior to the focus group work. Perhaps if this had been done these needs would have been prioritised and addressed.
Will this change the health of the nation?
It will all depend on how and who it’s communicated to and what behaviour change strategies will be put into place which as we all know, means funding. With Cameron’s Obesity Strategy expected to be announced in 2016, how much funding is put behind such campaigns will be the true sign of how seriously they are about tackling the health of the nation.
www.gov.uk/government/publications/the-eatwell-guide

by Nutrilicious | Feb 10, 2016 | Retail, Interviews
We recently worked with Waitrose on an exciting health and nutrition project where we truly saw the impact that a dietitian in retail can have on public health and sales. Moira Howie, Waitrose’s Manager in Nutrition and Health kindly agreed to tell us more about her journey. Here are the highlights.
When the opportunity to be a retail nutritionist came my way… I couldn’t resist. I knew that what people ate impacted their health so what better way to bring about changes than by helping to shape their weekly shopping basket. It sounds simple and easy but in reality the general public are quite resistant to change and those good intentions don’t always translate into practical action.
Adopting a multi-faceted approach to helping consumers choose a healthier diet yields the best results. The early creation of an online nutrition advice service containing a wealth of topical information helped to grow and build consumer trust in accessing sensible and practical advice. Consumers seem to struggle in getting information that meets their specific dietary needs therefore bespoke shopping lists are always in demand. New technology has changed the shape of this information from paper to screen to phone but the requests remain the same “help me know the things I can eat as opposed to the things I can’t!” This essence of practical help extends through all publications from inspirational recipe cards carrying our Living Well logo to weekly and monthly columns on topical health concerns. But communication in itself is never going to solve the wider public health problems.
The changes required are more fundamental ranging from policy to product. Developing nutrition policy and setting strategic direction to deliver the ambition is at the heart of what we do. Policy needs to reflect latest nutritional thinking and be commercially appropriate for the retail setting. This approach enables our business to play a key role in helping to reduce calories, saturated fat, sugar and salt – those nutrients of concern in the UK diet and also to set goals for increasing fibre, vegetables, fruit and oily fish intakes to help achieve dietary balance. The nutrition policy influences new product development, drives nutrition reformulation and helps our suppliers to create great tasting products.
While scientific recommendations provide us with the evidence and the numbers it is the translation of these into real foods for our shopping baskets and recipes for our family tables that will make the difference. Successive governments have a keen interest in a healthier population and recognise that collaborative working achieves more. The Public Health Responsibility Deal has overseen decreasing salt levels in the UK diet, introduced the ‘easy to use’ front of pack labelling system that is now the norm across much of the food industry. These are significant successes and retailing will continue this momentum to bring about similar changes which impact public health in a positive way.
Moira Howie February 2016
Manager, Nutrition & Health

by Nutrilicious | Feb 3, 2016 | Health Awareness Events, Hot Topics in nutrition
As weight-busting January came to an end it brought to light a new, hard-hitting report from the WHO Commission on Ending Childhood Obesity (ECHO), with the alarming headline that, globally-speaking, at least 41 million children aged under five years are obese or overweight (1).
Applying the emergency brake on obesity: Whose role is it?
Unsurprisingly, The ECHO report, based on a review of the evidence, highlights childhood obesity as a complex and multidimensional problem. However, according to the report, the greatest obstacle to effective progress on reducing childhood obesity is a lack of political commitment and a failure of governments and other actors to take ownership, leadership and necessary actions. The WHO calls on governments to take effective leadership on obesity by incorporating large-scale cultural environmental and behavioural change without which change simply will not happen.
The knowns
We know that obesity has a massive impact on a child’s quality of life, from physical as well as psychological perspectives; studies also show that obese children face significant risk of obesity in adulthood, which itself poses major health and economic consequences for families and wider society (2).
The report paints a bleak picture that the prevalence of children being overweight under the age of five has risen, from 4.8% in 1990 to 6.1% in 2014, or an increase of 10 million children. On closer scrutiny, the statistics reveal that the most significant change in prevalence has been in Asia and Africa, driven by globalisation and urbanisation leading to obesogenic environments. Another major driver highlighted was the marketing of ‘unhealthy foods and non-alcoholic beverages’ which feature heavily in the recommendations.
The answers
The report proposes a set of policy recommendations to address three strategic objectives:
- To tackle the obesogenic environment and norms.
- To reduce the risk of obesity during critical periods in the life-course —preconception and pregnancy, infancy and early childhood, and older childhood and adolescence.
- The provision of treatment for children who are obese to improve their current and future health. To unpack this further, six broad recommendations are highlighted:

1 Promote intake of healthy foods
Implement comprehensive programs that promote the intake of healthy foods and reduce the intake of unhealthy foods and sugar-sweetened beverages by children and adolescents.
2 Promote physical activity
Implement comprehensive programs that promote physical activity and reduce sedentary behaviours in children and adolescents.
3 Preconception and pregnancy care
Integrate and strengthen guidance for the prevention of non-communicable diseases with current guidance on preconception and antenatal care.
4 Early childhood diet and physical activity
Provide guidance on, and support for, healthy diet, sleep and physical activity in early childhood and promote healthy habits and ensure children grow appropriately and develop healthy habits.
5 Health, nutrition and physical activity for school-age children
Implement comprehensive programmes that promote healthy school environments, health and nutrition literacy and physical activity among school-age children and adolescents.
6 Weight management
Provide family-based, multi component, lifestyle weight management services for children and young people who are obese.
While the report highlights, the limited potential of any single intervention to provide a solution, within these overarching recommendations are more specific targets, focussed on tackling the obesogenic environment.
Targets for the food industry feature prominently. Within the first recommendation, there is a call to implement ‘effective taxation on sugar-sweetened beverages’ and to implement context-specific nutrition information, and ‘interpretive’ front-of-pack labelling. The food and drink industry, retailers and marketing stakeholders are called upon to clampdown on junk food marketing with the report recommending that advertisements for ‘unhealthy products’ should be banned from children’s TV, schools and sports facilities. Sizing up is also singled out as a particular issue to address and there is scope and opportunity for the industry to address appropriate portion sizes.
Schools also offer a key opportunity for action and the report’s recommendations focus on: standards for school meals; elimination of so-called ‘unhealthy foods’, such as sugar-sweetened beverages and energy-dense, nutrient-poor foods, in the school environment; informed nutrition education as part of the core curriculum; and ensuring levels of physical activity for all children, meet current recommendations, with comprehensive programmes that reduce sedentary behaviours in children.
Similarly, health professionals have a major role to play if the recommendations are to be in any way implemented which will take considerable investment in the work-force to achieve the skill-sets required, as well as the resources. The roles that schools and health professionals have to play can only be realised by ensuring that there are measures and funding in place to support them. Even before birth, the behavioural and biological responses of a child to the obesogenic environment can be shaped by processes (3). x7Hanson, MA and Gluckman, PD. Early developmental conditioning of later health and disease: physiology or pathophysiology?. Physiol Rev. 2014; 94: 1027–1076 CrossRef | PubMed | Scopus (30)See all References7 Having clear guidelines which start to tackle that environment is a starting point with independent research being used to show what works. This must start with giving schools and health professionals the support to run evidence-based interventions: for example, dietitians having a role in ante-natal settings to advise mothers-to-be on healthy diets for themselves, and as gatekeepers for the whole family; schools to have teachers who are able to deliver nutrition education as part of the curriculum, as well as giving space in the school environment for more movement. One of the recommendations is to ‘make food preparation classes available to children, their parents and caregivers’ – even to achieve this single measure, vast investment and training is needed.
Caterers also have a crucial role, especially those working within the public sector such as in schools and hospitals and early-years settings and are called upon to meet the recommendations to limit consumption of foods high in fat, sugar and salt; ensuring availability of healthy foods.
Getting to the known unknowns
Whilst some of the report’s recommendations are in place already in the UK, for example, the National Child Measurement Programme to help monitor weight changes http://www.nhs.uk/Livewell/childhealth1-5/Pages/ChildMeasurement.aspx the UK has yet to put in place resource for dealing with those found to be overweight as well as making recommendations for weight gain in pregnancy. Research priorities are needed so that the evidence is in place to make UK-specific recommendations. But, as the McKinsey report (5) highlighted, lack of research should not be a barrier to action.
So does accountability now lie within government versus local communities, individual responsibility etc? We have long known and as the ECHO report states ‘without joint ownership and shared responsibility, well-meaning and cost-effective interventions have limited reach and impact’. However, this joined up thinking and action has never happened and is unlikely to happen without clear co-ordinated leadership, appropriate powers and accountabilities with specific targets. Will Cameron now lead us with a ground breaking strategy for the UK that is lead right from the top with a COBRA style committee to truly address the nation’s health crisis in his forthcoming childhood obesity strategy? Will he be brave or will he leave it to his successors to sort out? No government has ever achieved this to date. Yet we have never needed it more than it is needed now. Let’s hope he has his eyes wide open on and the determination focus and foresight needed.
References
Commission on Ending Childhood Obesity. Report of the Commission on Ending Childhood Obesity. World Health Organization, Geneva; 2016 http://www.who.int/end-childhood-obesity/en/ (accessed Jan 29, 2016)
Litwin, SE. Childhood obesity and adulthood cardiovascular disease: quantifying the lifetime cumulative burden of cardiovascular risk factors. J Am Coll Cardiol. 2014; 64: 1588–1590
Hanson, MA and Gluckman, PD. Early developmental conditioning of later health and disease: physiology or pathophysiology? Physiol Rev. 2014; 94: 1027–1076
van Jaarsveld CHM, Gulliford MC. Childhood obesity trends from primary care electronic health records in England between 1994 and 2013: population-based cohort study. Arch Dis Child. doi:10.1136/archdischild-2014-307151
McKinsey Global Institute. Overcoming Obesity: An Initial Economic Analysis. McKinsey Institute; 2014 http://www.mckinsey.com/Insights/Economic_Studies/How_the_world_could_better_fight_obesity (accessed Feb 3, 2016)