by Tanya HAFFNER | Feb 23, 2018 | Media in context, The Nation’s Health, Surveys and insights
Popular in the news this week is the story linking eating ‘ultra-processed’ foods and cancer, as reported by the Independent (‘Processed food, sugary cereals and sliced bread may contribute to cancer risk, study claims‘) the BBC the Daily Mail and The Guardian.
These headlines are based on a study published in the British Medical Journal this month. In the study, foods were classified based on the NOVA system, which relates to the nature, extent and purpose of food processing. Those falling under the category of ‘ultra-processed’ include:
- Mass-produced bread and buns
- Sweet or savoury packaged snacks including crisps, chocolate bars and sweets
- Sodas and sweetened drinks
- Meatballs, poultry and fish nuggets
- Instant noodles and soups
- Frozen or shelf-life ready meals
- Foods made mostly or entirely from sugar, oils and fats
Study details and findings
A cohort of 105,000 people were followed for an average of five years. A 10% increase in the proportion of ultra-processed foods in the diet was associated with a significant 12% increase in the risk of overall cancer and 11% in the risk of breast cancer.
Alongside the original study, the British Medical Journal have also published an editorial further explaining the findings.
Behind the headlines: the Nutrilicious dietetic view
Limitations of the study
While this story has been heavily publicised, there are several limitations of the study which mean we cannot draw firm conclusions:
- Those who ate a lot of ultra-processed foods had other behaviours that have been linked to cancer which could skew the results. They include being more likely to smoke, being less active, consuming more calories overall and more likely to be taking the oral contraceptive. The researchers stated that their impact ‘cannot be entirely excluded’.
- Cause and effect cannot be established for an observational study: we cannot say that ‘ultra-processed foods have caused the increase in cancer’. It is an association found.
- The term ‘ultra-processed’ is still somewhat vague, so it’s difficult to establish which specific foods might be responsible for the increased cancer risk, and why.
- The participants were mainly women who had decided to take part in a health and diet study themselves, so were likely to be interested in their health. This means the sample may not be highly representative of the general public.
That said, we can give credit to the large sample size used in the study giving more reliability to the findings.
Response from Cancer UK
Helping to put this study into context, Professor Linda Bauld from Cancer Research UK responded: “It’s already known that eating a lot of these foods can lead to weight gain, and being overweight or obese can also increase your risk of cancer, so it’s hard to disentangle the effects of diet and weight.”
She also said the study was a ‘warning signal to us to have a healthy diet’ but individuals should not worry about eating a bit of processed food ‘here and there’ as long as they were getting plenty of fruit, vegetables and fibre.
So, can we reduce the risk of cancer?
It’s estimated that one in two people will develop cancer at some point in their lives. Whilst some risk factors for cancer are non-preventable (such as genetics), there are still lots of things we can do to help reduce our risk:
- Eating a healthy, balanced diet
- Limiting red meat and avoiding processed meats
- Maintaining a healthy weight
- Abstaining from smoking
- Keeping alcohol intakes below government guidelines
- Protecting your skin from sun damage
- Knowing your body (e.g. checking for lumps)
For more details on all of the above, go to the National Health Service. The World Cancer Research Fund also carry out a continuous review of the scientific evidence into the subject of diet, lifestyle and cancer risk. Read their cancer prevention recommendations.
Takeaway message
This study does not allow us to draw firm conclusions about ultra-processed foods and cancer. However, we should certainly be reminded of the importance of diet and lifestyle in cancer prevention.
After smoking, excess weight is one of the biggest causes of cancer and it has also been estimated that about one third of cancers could be prevented by changing our diet and lifestyle. This includes being a healthy weight, following a healthy diet and engaging in physical activity.
What changes could you make to help reduce your risk?
Reference: Macmillan Cancer and Cancer Research UK

by Tanya HAFFNER | Feb 19, 2018 | Thoughts, The Nation’s Health, Surveys and insights
Plant-based diets made the headlines again this week, with coverage of a study suggesting a vegan diet can prevent type 2 diabetes. It was reported by the Daily Mail (‘Going vegan can prevent overweight adults from falling victim to diabetes’) and Medical News Today.
In the study, 75 participants were put into two groups. One group was asked to follow a low-fat, plant-based vegan diet with no calorie restriction. The other was asked to make no dietary changes for a period of 16 weeks. Participants prepared all their own meals and for both groups, alcoholic drinks were restricted to one per day for women and two per day for men.
All the participants had a Body Mass Index (BMI) between 28kg/m2 and 40kg/m2 (putting them into the ‘overweight’ or ‘obese’ categories), with no history of diabetes.
At the end of the study, the plant-based group reported:
- Marked improvements in beta-cell functioning – these are the cells which produce the hormone insulin, which is important for controlling blood sugar levels (a key factor in diabetes where blood sugar levels are elevated or harder to control).
- A significant increase in how well the body responded to insulin – when the body is less sensitive to the hormone insulin, it increases the chances of developing type 2 diabetes.
- A decrease in BMI and body fat levels – this is important because excess body weight is strongly associated with increased risk of type 2 diabetes.
It was reported that neither group made any changes to their physical activity regimen, nor did they change the use of their medications.
Read more details of the original study
Behind the headlines: the Nutrilicious dietetic view
Whilst this is yet another study showing positive effects arising from a plant-based diet, we must be aware of its limitations:
- Efforts were made to help ensure adherence to the diet (such as dietitian telephone calls to the participants and food diaries completed at the start and end) but this still relies on the honesty and accuracy of the participant.
- As noted by the researchers, the participants used in the study were ‘generally health-conscious individuals’ who were willing to make significant dietary changes. Thus, we cannot be sure findings would be representative of the general population if they were to eat a vegan diet.
- The study is too short and too small to show conclusively that a vegan diet prevents type 2 diabetes.
- The meals were prepared by the participants and thus any changes or fluctuations were not controlled or recorded.
On the other hand, a strength of the study is that it was a randomised controlled trial, which is the gold standard in research for measuring the effectiveness of an intervention.
The link between plant-based diet and reduced risk of diabetes
The researchers recognised that the major factor accounting for the reduced risk of type 2 diabetes in the plant-based group was the weight lost (including visceral fat lost).
The link between the two is well established. Research shows that for every kilogram of weight loss, there is a 16% reduction in risk or type 2 diabetes.*
The generally higher fibre and lower fat content of plant-based diets (which also includes vegetarian diets) would be expected to be helpful in reducing the energy density, and thus total calorie content of the diet. This could help with reducing obesity.
*Hammam et al (2006) Effect of Weight Loss With Lifestyle Intervention on Risk of Diabetes.
Takeaway points
In the UK, 11.9 million people are at risk of developing type 2 diabetes: prevention is clearly of great importance. The disease can have both short-term and long-term complications.
Further research will be needed to determine whether a vegan diet could prevent type 2 diabetes, and whether the positive improvements noted in this study require a strict vegan diet or whether the positive effects could be achieved with smaller changes.
Evidence shows the best ways to reduce risk of type 2 diabetes include:
- maintaining a healthy weight;
- eating healthily; and
- keeping physically active,
Adopting principles from a plant-based diet can certainly help with the first two points. The range of benefits of adopting a more plant-based diet are discussed further in last week’s blog.
For more information on reducing risk see Diabetes UK alongside their useful information about veganism and diabetes.

by Tanya HAFFNER | Feb 16, 2018 | Hot Topics in nutrition, The Nation’s Health, Surveys and insights
The rise in popularity of vegetarian and vegan diets is in the news, including stories in the Daily Mail INews. This comes following a release by Kantar Worldpanel of supermarket sales figures and analysis of consumer behaviour. It revealed:
- Over January 2018, one in ten shoppers purchased a meat-free ready meal. This has increased by 15% compared with the same time last year.
- During January 2018, 29% of evening meals were now free of meat and fish.
- Britons consumed 3.9 billion meat free evening meals in the 12 months to October 2015. This rose to 4.3 billion in the 12 months to October 2017.
- As a nation, we consumed 87 million more entirely vegan-friendly meals in 2017 than in 2015.
Announcements of product sales and ranges underscore these figures. In just two examples, it was also reported in the news this week that sales of Quorn (a meat substitute product) have increased globally by 16%. Last month also saw Tesco bring out their own vegan range, Wicked Kitchen, highlighting the increasing demand for more plant-based options.
Behind the headlines: the Nutrilicious dietetic view
There are many reasons why we could be seeing an increase in the popularity of meat free meals.
The trend of ‘Veganuary’ (where individuals adopt a vegan diet for the month of January) is likely to have contributed to the findings which related to the month of January 2018.
Richard Allen, a spokesman for Kantar Worldpanel, emphasised increasing access to meat-free foods: “The surge in vegetarian evening meals over the past year is down to the wider availability of products which make eating meat-free more attractive and practical.”
He continued: “Our ideas about what’s healthy are also changing – we’re more focussed on foods that are natural and less processed and eating a varied diet.”
What are the benefits of a plant-based diet?
The evidence for plant-based diets is growing and can offer many benefits. Indeed, the updated ‘Eatwell Guide’ saw that plant sources of protein were listed ahead of animal food sources of protein. The protein group now has the title ‘Beans, pulses, fish, eggs, meat and other proteins’, highlighting the increased role plant-based diets can play.
Benefits of adopting a more plant-based diet include:
Health
- Research has shown that vegetarian and vegan populations tend to have lower blood pressure, cholesterol levels and rates of cardiovascular disease compared to their omnivorous counterparts. This could be due to less saturated fat in the diet and more polyunsaturated fats, in addition to other cardio-protective components in the diet such as soya and nuts.
- Plant-based diets tend to have a more balanced macronutrient profile. For example, the higher fibre content of plant-based diets is often accompanied by lower fat intakes. This can help reduce the energy density of the diet and thus help reduce the total energy (calorie) intake. This could help prevent people being overweight/obese, and therefore any related negative effects and co-morbidities (e.g. type 2 diabetes, increased cancer risk etc).
Environment/sustainability
- Animal foods are resource intensive (energy, land and water) and thus tend to have higher greenhouse gas emissions compared to plant foods per unit weight.
- Modelling work has shown that reducing the amount of animal foods in the diet will make a critical contribution to climate change mitigation.
Economic
- Recent research has suggested that the British government could reduce its healthcare and societal costs by £5.21 billion if just 10 per cent of the UK population emphasised plant-based foods in their diet.
References: Clarkson V, Plant Food Sources of Protein for Optimum Health, Muscle Status and Sustainability – The Evidence and Practice and Schepers J & Annemans L., The potential health and economic impact of plant-based food patterns in Belgium and the United Kingdom. Nutrition 15th December 2017 (in press)
Does this mean meat is off the menu?
Gaining the benefits of a plant-based diet does not have to mean a diet no with meat at all. A ‘flexitarian‘ diet is predominantly plant-based without completely eliminating meat and can be extremely beneficial for health and reducing carbon footprints.
Indeed, meat, poultry and fish are nutritious foods and can provide a range of nutrients beneficial for health. We are advised by the NHS to have two portions of fish per week, one of which is oily. They also advise how meat can fit into the diet.
Takeaway points
We welcome findings that plant-based meals are being explored and becoming more popular. We encourage everyone to enjoy a varied diet featuring a wide variety of plant-based whole foods.
Overall, plant-based eating isn’t new. It’s not radical. And it’s definitely not about cutting things out. A plant-based diet shouldn’t be defined by what it excludes, but by what it includes. The core message is ‘put plants first’. Instead of planning meals around meat, bring veggies, fruits, whole grains, pulses, legumes, nuts and seeds from the side of the plate to front and centre.
It doesn’t have to be wholesale change: many benefits can be achieved by simply reducing intake of meat rather than following a strict vegetarian or vegan diet. We recommend making small steps to include more plant-based foods and meals in your diet, to benefit your health and the planet.
If you do decide to go further, the NHS gives advice on ensuring a vegetarian or vegan diet is balanced. The British Dietetic Association are part of an important alliance with the Vegan Society to share the message that all well-planned vegan diets can support healthy living in people of all ages.

by Tanya HAFFNER | Feb 9, 2018 | Hot Topics in nutrition, Media in context, Surveys and insights
Each week we investigate the nutrition and diet topics making the headlines. This week, the Daily Mail discussed the health profiles of non-dairy milk alternatives.
The article was based on a study in the Journal of Food Science and Technology titled ‘How well do plant-based alternatives fare nutritionally compared to cow’s milk’?
The four most consumed non-dairy milk drinks were studied: almond, soy, rice and coconut milk (all unsweetened varieties). Nutritional values were obtained from the food packaging and the USDA database.
The review discussed the pros and cons of each milks, with the aim to help make consumers be able to make a more informed decision. Their main findings were as follows:
| Coconut milk |
Almond milk |
Rice milk |
Soya milk |
Pros
Low calories
Taste
Cons
No proteins
Rich in saturated fats |
Pros
Balanced diet
Low calories
Taste
Cons
Almond allergy |
Pros
Comparable caloriesCons
Rich in sugar
Unbalanced diet |
Pros
Rich in protein
Balanced dietCons
Taste
Soy allergy |
The headlines point to soya is the best alternative to cow’s milk, with researchers concluding that, ‘among alternative milks only soy milk contains comparable amounts of nutrients’.
More detailed findings and rationale for each of the points above are all discussed in the original study, alongside nutritional values for each of the milks.
Behind the headlines: the Nutrilicious dietetic view
The study is especially relevant because of the increasing popularity of non-dairy alternatives to milk and the increasing recognition of the health benefits of plant-based diets, and plant foods being more environmentally sustainable. Indeed, the latest ‘Eatwell Guide’ from Public Health England updated the name of one of the food groups from ‘Milk and Dairy Foods‘ to ‘Dairy and Alternatives’, highlighting the growing role of such foods in our diets. Plant food sources of protein were listed ahead of animal food sources of protein for the first time: the protein food group is now called ‘beans, pulses, fish, eggs, meat and other proteins’.
See our blog on the new Eatwell Guide
There are many reasons why people are choosing such products, including health, environment, allergies and intolerances, and veganism.
Our assessment of the study
- A good amount of data was analysed. For a non-dairy milk to be included within this study, at least four examples had to be available for each type of milk.
- The study uses American data. We cannot be sure findings will be the same for the UK and Irish products, although they are likely to bear many similarities. Opinions were also gathered regarding taste of the different milks and the UK population may react differently.
- Due to missing data, the research did not cover all the vitamins as intended.
One of the main conclusions from the study was that soya milk contained more protein than other alternatives. We did our own analysis of the four unsweetened* milks, alongside two other unsweetened milks available for reference. Here are our findings:
|
Cow’s milk (Semi skimmed) |
Coconut milk |
Almond milk |
Rice milk |
Soya milk |
Oat Milk |
Cashew milk |
|
Per 100ml (mean values) |
|
|
| Energy, kcal |
47 |
36 |
13 |
47 |
29 |
40 |
26 |
| Fat g |
1.8 |
1.5 |
1.1 |
1.0 |
1.5 |
1.0 |
1.0 |
| Sat fat g |
1.1 |
1.4 |
0.1 |
0.2 |
0.3 |
0.1 |
0.2 |
| Sugars g |
4.8 |
3.3 |
0.1 |
6.2 |
0.5 |
3.7 |
1.7
|
| Protein g |
3.6 |
0.2 |
0.5 |
0.1 |
2.7 |
0.7 |
0.5 |
| Calcium mg |
123 |
120 |
120 |
120 |
120 |
120 |
120 |
| Vitamin D2 ug |
0.00 |
0.75 |
0.89 |
0.89 |
0.75 |
0.75 |
0.75 |
| B12 ug |
0.91 |
0.38 |
0.38 |
0.38 |
0.38 |
0.38 |
0.38 |
Values from Forestfield Dietplan 7, National Dairy Council – the nutritional composition of dairy and plant-based drinks nutritional information: a range of current products on the market. *There are also sweetened versions of these products on the market.
Is soya milk the best non-dairy alternative?
- Protein The most notable similarity between cow’s milk and soya milk compared to the other non-dairy milks is the higher protein levels, as highlighted in the original study. While this has grabbed the headlines as being highly beneficial, for the majority of the UK population protein intakes are in fact in excess of requirements. The UK National Diet and Nutrition Survey shows that only 7–8% of protein for those aged 11–65+ comes from cow’s milk. Calling one milk ‘healthier’ than the other based on this alone is generally not useful or appropriate. Single food measures of protein content or indeed quality do not reflect the scale of impact across the total diet and not enough attention is given to this key consideration.
- Calcium Cow’s milk is known to be a great provider of the UK’s calcium intake, providing from 26% in 4–10 year olds to 18% in 11–18 year olds and in 19% in adults aged 19–64. We can see that all of the non-dairy alternatives to cow’s milk closely match this. They are also fortified with vitamin D, which aids in calcium absorption and is beneficial for bone health. Cow’s milk in the UK does not have vitamin D.
- Saturated fat One benefit of all the non-dairy milks is that they are generally lower in saturated fat than cow’s milk, providing 0.1–0.6%. Coconut milk is the exception, with levels higher at 0.9–1.9%. One 200ml glass of coconut milk provides 2.8g saturated fat on average, whereas the other non-diary milks average at 0.4g saturated fat. The coconut milk ranks ‘medium’ for saturated fat under the drinks traffic light labelling system, the others are ‘low’.
- Cholesterol Looking more specifically into soya and the advantages it can have for health, one point not discussed in this study is that soya can also help reduce cholesterol levels. This forms part of the Ultimate Cholesterol Lowering Plan from HEART UK.
- Iodine This essential trace element is an important component of the thyroid hormones. A recent study from the University of Surrey investigated 14 non-diary milks in the UK and found that iodine levels were only 2% that of in cow’s milk. Women of childbearing age and pregnant women are most at risk of deficiency. Information on alternative sources of iodine are discussed on a British Dietetic Association (BDA) iodine factsheet.
- Is soya ok? Soya products such as soya milk alternatives often hit the news, with suggestions they can be bad for our health. However, many of these claims are untrue, as discussed on the BDA Fact Sheet for Soya. Soya forms part of a healthy balanced diet. The British Heart Foundation also discusses the role of soya milk as a replacement for cow’s milk. A very recent review of plant food sources of protein for optimum health by Dietitian Vanessa Clarkson can be found on this plant protein fact sheet
Conclusions
A healthy alternative for adults
For those looking to replace cow’s milk in the diet with a plant-based milk, fortified soya milk bears the most nutritional similarities to cow’s milk. However, the other plant-based drinks analysed also provide many of the nutrients. Its crucial to consider them in the context of the whole diet and we feel confident that these products can contribute to a healthy balanced more plant-based diet for adults.
Which non-dairy milk is considered the ‘best’ will depend on individual needs, with personal taste playing an important role. Faced with so much choice, here are some points to consider when buying a non-dairy alternative to milk:
- Choose non-dairy milks that have been fortified with calcium and vitamin D for bone health. Organic varieties and homemade milks may not contain high enough levels – read the label.
- For vegans in particular, choose a milk that has been fortified with vitamin B12 – often found to be low in the vegan diet. Other groups at risk of low vitamin B12 including vegetarians, the elderly and individuals with gastrointestinal disorders.
- Choose unsweetened varieties where possible to minimise intake of free sugars.
- Soya milk is higher in protein than other non-dairy alternatives, although lower protein milks should not pose an issue for the general adult population.
- Soya milk can help as part of a cholesterol-lowering diet.
- Coconut milks will be higher in saturated fats, which can raise ‘bad’ LDL cholesterol levels.
- Swapping cow’s milk for non-dairy alternatives could result in a lower iodine intake unless the milk has been fortified with iodine. Some may be fortified – read the label if there is a concern.
- As with any food or drink product, don’t just treat it in isolation: it’s the total dietary intake that’s important. Whether having dairy milk or a substitute, we need to make sure that our overall food intake is healthy and nutritionally balanced.
Non-dairy milks for children
Parents of children wishing or needing to avoid cow’s milk should seek dietetic advice to ensure their diet is balanced at every age. See the British Dietetic Association factsheet for more information
.

by Tanya HAFFNER | Dec 15, 2017 | Surveys and insights, Changing mindset, Impactful health initiatives, Resources worth having
Currently 2.3 million people in the UK are living with heart disease, at an annual cost of £953m to the NHS. We’re involved in an on-going battle to try to reduce it.
For those in the health industry, the link between high cholesterol and heart disease is well known. Meta-analyses, genetic studies and randomised controlled trials totalling more than 2 million participants, 20 million person-years of follow up and 150,000 cardiovascular events demonstrate a close correlation between cardiovascular disease (CVD) and high levels of low-density lipoprotein cholesterol (LDL-C).
What’s less known is the impact plant stanol esters can have on lowering cholesterol.
Changing behaviours of those at risk of heart disease
GPs and practice nurses are key influencers when it comes to persuading people to change their lifestyle to improve their health. So it’s vital to make sure these healthcare professionals (HCPs) have the facts – and materials – they need to support this.
In a survey we undertook this year of HCPs on behalf of Benecol, we found that persuading patients to improve their diet change is a key priority when it comes to reducing cholesterol – along with cutting smoking and increasing physical exercise.
We discovered that while the HCPs are well aware of the importance of cutting saturated fat and sugar, and want to communicate about healthier eating to patients, they are less likely to know the impact plant stanol esters can have on lowering cholesterol.
Plant stanols and sterols can reduce cholesterol by up to 10% in two to three weeks.
Over 70 clinical studies have demonstrated that plant stanols effectively lower cholesterol.
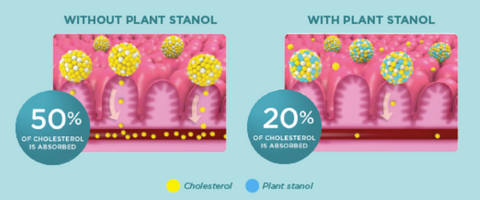
How do they work?
Consumption of foods with added plant stanols or sterols (1.5 – 2.4g/day) should take place at meal times. Mixing with food and digestive juices results in the displacement of dietary and biliary cholesterol in the fat absorption pathways in the gut.

Cholesterol absorption is reduced by about 50% and studies have shown a dose-dependent reduction in circulating LDL-C of 7 – 10% on average.
Cholesterol begins to lower immediately. With continued use full reduction is achieved within 2 – 3 weeks and is sustained over the longer term. What’s more, if used alongside statin therapy, plant stanols lower LDL-C by an additional 10% – an effect greater than doubling the statin dose, which, at best, only provides a 6% additional LDL-C reduction.
Plant stanols provide an easy diet-based solution to all hypercholesterolaemic patients, including those with mildly elevated serum cholesterol level. They would also be especially recommended for those averse to taking statins, anxious to keep statin doses low, or at higher risk from potential statin-related side effects.
They are recommended by a number of prevention and treatment guidelines as part of a cholesterol-lowering diet, including the European Society of Cardiology, the Atherosclerosis Society, UK JBS3 guidelines and the World Health Organisation.
Our holistic communications approach to help reduce cholesterol
As a result of our research, we created a holistic communications approach in association with HEART UK – the Cholesterol Charity and leading heart health dietary specialists – to support practice nurses and GPs, and their patients.
- We created information sheets for the healthcare professionals with full information about dietary changes patients can make to lower LDL-C levels. Included in this was the latest evidence not only on plant stanols but on all dietary recommendations for lowering LDL-C.
- Alongside this were fact sheets for patients, clearly explaining the problem of high cholesterol and the lifestyle changes that would have a significant impact on their health.
We highlighted the key motivators for patients – the fact that a small change would bring quick results.
Companies are accused of only being interested in their profits – and of course, they are ultimately accountable to stakeholders, so money is always going to come into it.
But what we found with Benecol’s approach is that they are genuinely determined to help combat the huge problem of heart disease that exists. Reaching out to health professionals they wanted to understand issues fully and how best to communicate lifestyle change – not just dietary, which would help promote the message of plant stanols, but also more widely, include all dietary matters as well as smoking and exercise.
The materials tell the whole story, educating the professionals and patients and then leaving it in their hands how to act.
Health professionals responsible for communicating heart health cholesterol lowering advice can order these packs by calling the Benecol Helpline 0800 018 4010 and asking for your health professional Benecol Toolkit ‘Small Change, Big Results’ pack.

by Tanya HAFFNER | Dec 4, 2017 | Retail, Food category comment, Media in context, The Nation’s Health, Surveys and insights
Each week we analyse some of the hot headlines in health and nutrition news. This week cheese; obesity & diabetes/cancer risk; and sugar reduction in Kellogg’s cereals.
HEADLINE 1: A piece of cheese a day keeps the doctor away
Picked up in the news this week by the Daily Mail, The Express, The Sun, The Independent and The Guardian is the suggestion that eating cheese could reduce the risk of heart attacks and strokes.
This is based on a meta-analysis of studies which concluded that consuming 40g of cheese per day reduced the risk of heart attack by 14% and stroke by 10%.
Behind the headlines: the Nutrilicious dietetic view
While cheese lovers are likely to have rejoiced, there are limitations to the research on which the headlines were based. The lack of randomised controlled trials included within the meta-analysis means that no causal relationship can be assumed between eating cheese and risk of heart disease. There are far too many factors which could interfere with the results.
Interestingly, there are previous large studies that have found no association between heart disease and eating cheese. Again, it can be hard to prove that it is the cheese eating that is causing the effects.
The harm that eating too much cheese can cause to health is well documented. Although it is a good source of protein, calcium, phosphorous and vitamin B12, it can also be high in saturated fats. Having too much saturated fat in the diet can increase levels of LDL cholesterol in the blood, which is an established risk factor for heart disease. A 30g portion of cheddar cheese (a matchbox size) contains 6.5g saturated fat (over a quarter of the reference intake for saturated fat – 20g). It can also be quite easy to go above this recommended portion size.
Some cheeses can be high in salt and there is a lot of evidence to show that too much salt can increase the risk of high blood pressure, another risk factor for cardiovascular disease.
Cheese can be enjoyed as part of a healthy diet if eaten in moderation and can provide a valuable source of various nutrients. Sticking to the recommended 30g portion size and opting for lower fat varieties such as lighter/reduced fat cheddars, cottage cheese and ricotta, can help ensure we don’t exceed our recommended maximum amount of saturated fat.
Moreover, foods such as low-fat yogurts and lower fat milks can also provide us with calcium and protein (two of the key nutrients found in cheese) but provide less saturated fats (as well as fewer calories, which would be helpful for those trying to lose weight).
For more information, go to British Heart Foundation and the NHS
HEADLINE 2: Diabetes is a key factor in WORLDWIDE cancer surge
The Express, The Sun and The Daily Mail reported on a finding that diabetes and obesity have been linked to causing cancer.
Researchers found that people with a high BMI (defined as above 25kg/m) who also had diabetes were behind 5.6% of new cancer cases globally, affecting 792,600 people in 2012. The method used was through assessing the increase in new cases of 18 cancers based on the prevalence of diabetes and high BMI in 175 countries (using data about BMI and diabetes in 2002 and cancers recorded in 2012).
Behind the headlines: the Nutrilicious dietetic view
This is an interesting study as it is the first study to have looked at the combined effect of having diabetes and obesity on cancer risk. Whilst the headlines alert us to the finding that over 5% of cancers were attributable to diabetes and cancer, there were significant differences between various groups of people, regions and types of cancer which should be noted. These are discussed in the original study. For example, cancers attributable to diabetes and being overweight were nearly twice as common in women (496,700 cases) as they were in men (295,900 cases).
It should be noted that there were limitations of the study. It is questionable whether the 10-year gap used between recording diabetes and high BMI to cancer incidence is entirely appropriate to enable conclusions to be drawn, as recognised by the researchers.
What we understand already is that obesity is certainly a risk factor for cancer. Analysis conducted by the World Cancer Research Fund has found that being overweight (BMI 25kg- 29.9/m) or obese (BMI 30kg/m and above) increases the risk of 11 types of cancer.
The Diabetes UK website outlines the link between diabetes and cancer. Some of the complications associated with diabetes can increase the risk of cancer. However, well-managed diabetes can help reduce the risk of any complications. Diabetes UK have given their thoughts on this study and stated that, “Diabetes doesn’t directly cause cancer, but this study adds to the evidence that having diabetes can increase the risk of certain types of cancer.”
The main message to take home from these headlines is that the increasing prevalence of obesity and diabetes may lead to an increase in risk of certain cancers. Maintaining a healthy weight, eating well, keeping physically active, not smoking, and not exceeding the government guidelines for alcohol consumption can all help lower the risk of diabetes and cancer.
For more information, go to Diabetes UK and WCRF
HEADLINE 3: Kellogg’s to cut sugar in kids’ cereals by up to 40%
Also in the news this week is the announcement that Kellogg’s will cut the sugar levels in children’s cereals by up to 40%. This was reported by the BBC, the Daily Mail, the Evening Standard, The Times and The Sun.
Kellogg’s have said they will reduce sugar levels by 20-40% by the middle of 2018 for Coco Pops, Rice Krispies and Rice Krispies Multi-Grain Shapes. They are also going to stop making Ricicles from January 2018, due to the amount of sugar in the cereal, and are putting a stop to on-pack promotions aimed at children on Frosties.
Behind the headlines: the Nutrilicious dietetic view
This is a very positive and encouraging move from Kellogg’s as the battle to reduce sugar consumption in the UK continues.
In March this year, officials at Public Health England called on food firms to cut sugar by 5% by the end of this year and by 20% by 2020. The Scientific Advisory Committee on Nutrition currently advise that free sugar intake in the UK should account for no more than 5% of our daily energy intake. Advice for the different age groups is as follows:
- Children 4-6 years – no more than 19g free sugars per day (5 teaspoons)
- Children 7-10 years – no more than 24g free sugars per day (6 teaspoons)
- Children 11 years + and adults – no more than 30g free sugars per day (7 teaspoons)
Although not the highest source of sugar in our diets, cereals do contribute to daily intake, with the most recent National Diet and Nutrition Survey highlighting that cereals are responsible for 5% of the added sugar intakes of adults and 6-8% of that of 4-10-year olds and teens. In our blog post last year A Health Check on New Breakfast Opportunities we discussed the need for more breakfast options to offer lower sugar choices and so this certainly is a positive step forward. With gradually a lesser number of options available that are high in sugar, it may be less overwhelming for consumers to make healthier choices.
Here is how much sugar is currently in the Kellogg’s products and how much they are to be reduced by:
- Coco Pops – 9g sugar per 30g serving. To be reduced to 5.1g per 30g serving (40% reduction, changing from about 2 teaspoons of sugar to just over 1 teaspoon).
- Rice Krispies – 3g sugar per 30g serving. To be reduced to 2.4g per 30g serving (20% reduction, changing from ¾ teaspoon of sugar to a little under 2/3 teaspoon of sugar).
- Rice Krispies Multi-Grain Shapes – 6.3g sugar per 30g serving. To be reduced to 4.5g per 30g serving (30% reduction, changing from about 1.5 teaspoons of sugar to just over 1 teaspoon)
A step forward to reduce the sugar content of any foods available on the market can only surely be a positive one.
For more information, go to Kellogg’s – Sugar and Breakfast Cereal and SACN 2015 – Carbohydrates and Health Report