by Tanya HAFFNER | Jan 23, 2020 | Thoughts, Changing mindset, Event Reports
What’s going to have the most impact on reducing sugar consumption in the UK – educating consumers and encouraging them to change their habits, or changing the environment, reformulation and marketing? Is responsibility ultimately on the individual or industry?
That’s one of the key questions that came out of a panel discussion I was part of at an Action on Sugar event held at Parliament for Sugar Awareness Week.
Campaigners, government officials, health experts and industry experts came together for a networking opportunity all wanting to make a difference, before sitting down to hear from our host Andrew Selous MP, who’s served on the Health Select Committee; Katherine Severi, Chief Executive of the Institute of Alcohol Studies; Professor Graham MacGregor, Chairman of Action on Sugar; and me, asked to speak about how sugar reduction can improve the health of the most vulnerable and what’s our view on industry’s role.
The theme of this year’s Sugar Awareness Week is ‘What’s in your drink’. Action on Sugar have done an excellent job at highlighting a loophole in regulations whereby alcoholic drinks are not obliged to label any nutritional information about their products – even though the calorific and sugar levels are often alarming.
There was universal agreement in the room that something must be done – and everyone can play their part by emailing their local MP to demand change. You can find lots more information on the Action on Sugar website, and I highly recommend you do so.
What, though, will be the ultimate impact of labelling? As Professor MacGregor said yesterday, although labelling and education are a vital step, it’s the environment, formulation of products and marketing that will truly have an impact.
As a nation we are consuming too much sugar on average, which can often mean too many calories, leading to weight gain and obesity. Children, our most vulnerable group, are consuming more than double their maximum recommended allowance of sugar.
In England, around 1 in 4 children have tooth decay and 1 in 3 are overweight or obese by the time they leave primary school.
What’s more, as a 4-5 year old, you’re three times more likely to be overweight or obese if you’re in the most deprived socio-economic group compared to the least deprived: 27.2% vs 17.3%. The results are even worse for 10-11 year olds.
Andrew Selous shared what he discovered on a learning visit to Amsterdam, where the mayor was inspired to do more to reduce child obesity after seeing a girl in a playground who was too overweight to do a forward roll. As the mayor pointed out, if one third of children were suffering from tuberculosis, there would be no avoiding the issue. Action would be taken. The army would be out on the streets helping.
Yet the with obesity comes the complex problem of stigma, shaming and how best to deal with the issue in a ‘publicly correct’ way that’s not going to impact mental health.
What is the role of the wide food industry, retail and out-of-home sectors?
Of course, consumers should make their own choices – and of course we want to encourage them to make good, informed choices benefiting their health and the planet where support for this must continue.
But numerous reports, behavioural change groups and experts globally all concur that if we leave things to individual choice alone, we will not achieve the behavioural change we need to see. We live in environments that are swamped with foods that are high in calories, fat, salt and sugar which are also low in protective nutrients and are heavily promoted to us. Industry has a crucial role to play in providing and marketing healthier choices. Industry can no longer blame poor eating habits on the consumer and their personal choice. It’s especially important for the vulnerable groups, who need the most help.
Examples of positive action for change
An inspiring example from Amsterdam was a supermarket who decided that they didn’t want their consumers to eat unhealthy foods. They changed their environment, made healthier food more accessible, reduced the amount of unhealthy products and made sure the labelling was clear. They had a profit to make but – led by the top – decided that the health of the public was their responsibility too.
Katherine Severi pointed to the action in Scotland to price alcoholic beverages based on the number of units they contained. A 3-litre bottle of cider that previously cost £3.50 went up to over £11 when the law was introduced in May 2018, making it far less accessible to the most deprived.
While it’s too early for full data analysis of the impact, early signs are extremely positive on the positive impact the pricing can have.
What are our recommendations to industry?
1. Stick with the sugar reduction despite the challenges (and ultimately you may have no choice). It makes sense and it’s vitally important to continue to see small subtle incremental reductions in sugar and calories. Reformulation takes time but it IS achievable – we have a precedent with salt reductions.
2. Have a nutrition and health strategy with teeth. It must be:
- Led from the top
- Long-term
- Multi-faceted
- Consistent and joined up across departments and suppliers
- Measured
- Aligned to both health and sustainability
- Communicated and understood right across the business – from CEO to porter
Marketing and external communications should focus on healthier choices, and for optimum impact should incorporate smart partnerships.
We can’t ignore that change has its challenges:
- Industry has to make money. We can’t impact on jobs in these vulnerable times
- There will be growing pains and these need to be listened to, carefully considered and supported
- Change takes time, goodwill and, crucially, support from the top
But there is reason to believe that now, perhaps, there are colliding drivers to move us in the right direction:
- The health of the nation and its impact on socio-economics is stark
- More and more consumer groups are demanding action, for both health and environmental issues
- The financial necessity to change is on the horizon. The likes of Share Action, amongst others, are telling investors that if business don’t change, they will be at risk.
Getting the government to take action
The government said they wanted to half childhood obesity by 2030. That is not going to happen with their current plan.
If our new Government doesn’t have the foresight to act and create the level playing field that industry says it needs, industry needs to get together and lobby for it to be implemented over a reasonable period of time, which at the very least:
- Ensures only healthy products (not high in fat, salt and sugar) to be marketed, promoted and advertised
- Makes uniform colour-coded labelling on front of pack mandatory on all products sold in retail and out-of-home
At the moment, despite all the health and economic imperatives, obesity simply isn’t the top of the agenda.
As each member of yesterday’s panel said, for the sake of our nation’s health and the planet, it’s going to take us all coming together to create a powerful voice and movement for change.

by Tanya HAFFNER | May 15, 2019 | Retail, Hot Topics in nutrition, Thoughts
My first SMART SHOP 🛒 ever!
A taste of the future of grocery shopping! 🍏 🍊 🥛
Have you experienced it yet? If so how was it? This is my short story….May 2019!
“I can do this”…I told myself as I hear my forever forward thinking colleague Howard @see_research tell me that @Sainsburys @SainsburysNews have a new smart shop in Holborn – must be tried!
Forget ones inbuilt fear about new tasks I tell myself, especially new tech tasks….which is always a slow learn for me, where I normally have to do things 2-3 times before it clicks! Instead, need to muster all life skills accumulated over many years to overcome said fear, gain new experience, stay ahead & be more informed about retail advances!
Swapping 👠 for 👟 after our meeting I bounce over to the new store with curiosity & best enthusiasm possible for joining in…thankfully greeted by helpful friendly young millennial providing immediate, necessary, app set up assistance & source of calm!
After 10 mins setting up the store app on my 📱 (not as easy as I had hoped with millennial help but thankfully unlike the much slower paced android next to me 😢 ) I was finally ready to go & shop like I never shopped before & looking forward to experiencing no checkout & a speedy exit!
I watched & copied those before me! I test scanned an 🍏 . I scanned the bar code on the apple shelf, then picked up the apple & placed it in my bag. Easy! “Whoopee” I say when camera scans it immediately. I briefly remind myself of a talk at my sons school the week before which inspired me to embrace tech +++ + as our near future is artificial intelligence in every which way possible. Suddenly feeling more positive about my chances with that! What fun! 😀
Onto the next shelf I tried to scan the bar code on the shelf in front of a pack of mixed fresh beans. Error appears! 😆Oh dear. You have to fail before you really succeed, right?! I discover that for packaged goods you have to scan the bar code on the pack – not the shelf! A little awkward & challenging when holding the product & my shopping bag & in need of at least one whole hand to take the scan on the iPhone & another hand to hold the product. But must not be defeated!
I scan two more items successfully. I then suddenly think about my next meeting & the need to run. I smugly look at the long queue in front of me & start to proceed to check out & pay on the spot on my app & search for the QR code on the shop wall to indicate Im done & leaving. Only snag….my apple pay linked to the app doesn’t accept @Barclays @BarclaysUK debit cards yet ,which explains the difficulties that even my helpful millennial did not realise at set up!
A bit frustrating having to leave & not complete the new task- but having no time for the store queue the store manger kindly takes my items back.
I did however leave thankful to @Sainsburys overall for the new shopping experience. It was of course a faff to set up the app even for the millennial assisting me and it obviously has a teething problem with some banking cards. However, once set up & you know where to scan I can only imagine it becoming second nature to us all very quickly.
On the negative side I can see us having no human contact as we go out to shop which adds to my concerns about the deterioration in social skills as tech inevitably increases in our lives. A big responsibility for the big tech corporations & us all to address, I think.
On the positive side I can visualise all kinds of new nutrition tech supporting this app that may analyse our shop as we scan, potentially feedback to us as we shop & help nudge us towards healthier & more sustainable shopping baskets! How amazing would that be!
Watch this space… I have no doubt! If you have experienced smart shop or have any further thoughts Id love to hear! In the meantime happy 😃 healthy shopping everyone however you choose to do it right now! 🛒

by Tanya HAFFNER | Jan 25, 2019 | Hot Topics in nutrition, Surveys and insights
“The world’s diets must change dramatically,” said Harvard University’s Walter Willett, one of the leaders of the comprehensive EAT-Lancet report released this week researching healthy and sustainable diet.
The findings show we must drastically cut down on meat and dairy, and eat more plant foods.
Published after three years of reviewing extensive evidence from around the world, the message is similar to that of both the British Dietetic Association’s One Blue Dot campaign, the government Eatwell Guide, the World Health Organisation and recommendations made by various non-governmental health organisations, for example World Cancer Research Fund (WCRF) and the British Heart Foundation.
The EAT-Lancet recommended daily diet
Here’s an outline of the recommended daily diet to meet 2,500kcal and all micronutrients:
|
Average recommended intake* |
Comment
|
| Daily |
Weekly |
| Protein foods |
| Beef, lamb and pork |
14g |
98g |
· Less than a quarter pounder per week
· Significantly below the WCRF recommendations of 350-500g per week
· 70-90% below current US & European intakes |
| Chicken and other poultry |
29g |
203g |
· Equivalent to around 1½ chicken breasts per week
· EAT suggests that the poultry allowance can be exchanged for eggs, fish or plant proteins and vice versa |
| Eggs |
13g |
91g |
· Equivalent to around 1½ eggs per week |
| Fish |
28g |
196g |
· Around 1½ – 2 servings a week
· Oil rich fish is strongly recommended as an omega-3 source |
| Legumes: dry lentils, beans, peas & soya foods |
75g |
525g |
· Equivalent to roughly 150g cooked / tinned beans daily
· An allowance within the 75g recommendation for soya products is specified due to the association with lower breast cancer incidence and reduced cholesterol levels |
| Tree nuts & peanuts |
50g |
350g |
· Equivalent to 1½ handfuls daily
· The report acknowledges that some nut and legume crops use intense water farming. However, the evidence for their associated reduced cardiovascular disease, cancer and total mortality risk justified this environmental trade off. |
| Dairy |
| Milk or equivalent in cheese / yogurt etc. |
250g |
1.75L |
· This is a significant reduction in dairy recommendations |
| Carbohydrates |
| Rice, wheat, corn and other, dry weight |
232g |
1.62kg |
· Whole grains advocated
· Equivalent to 1 servings of rice or pasta, 40g serving of breakfast cereals & 2 large slices bread daily |
| Tubers or starchy vegetables |
50g |
350g |
· Equivalent to 1 egg-sized potato daily or 1½ baked potatoes weekly |
| Non-starchy vegetables |
| All vegetables |
300g |
2.1kg |
· Notably, more vegetables than fruit recommended
· 3-4 servings daily |
| All fruits |
200g |
1.4kg |
· 2 servings daily |
| Added fats |
| Unsaturated oils |
40g |
280g |
· Equivalent to 4tbsp oil daily |
| Saturated oils |
≤11.8g |
≤83g |
· An allowance was made taking into consideration using all animal parts
· Equivalent to a single butter pack |
| Added sugars – no more than 5% energy intake – approx. 30g or 7tsp per adult per day. |
* EAT-Lancet recommended diet as well as an average daily intake, also provides a range of intakes.
Some of the notable findings are around red meat for iron and dairy for calcium:
- Iron: There is a problem with deficiency for adolescents but encourages use of inexpensive supplements over consumption of red meat
- Calcium: The United States and other countries over-estimate calcium needs. It is ubiquitous in the diet and there is little evidence that intakes above 500mg per day improve bone health.
The report looks how to change people’s choices to include less meat/dairy, through:
– making healthier foods more accessible and more cost effective
– reducing marketing and availability of unhealthy food.
It also tackles farming changes to a high degree – seen as being as important as, if not more than consumer change.
Conclusion? Change is needed, it’s going to be tough
We need to make big changes in our eating patterns if we’re going to protect our planet and health. It requires a multi-system combined effort approach to reduce food waste/losses, improve food production and encourage dietary shifts.
It is time for everyone to be involved in the urgently-needed transformation of our food system. We’ll be monitoring the impact the report has over time. Stay tuned…

by Tanya HAFFNER | Jan 17, 2019 | Hot Topics in nutrition, The Nation’s Health
What’s hot in the wacky world of wellness in 2019
Historians believe that the practice of New Year resolutions originated in the Babylonian Kingdom, over 3,000 years ago. New Year intuitively brings time for pause, reflection and setting intentions for the year, and for many, that can centre on resetting what they eat, especially after indulging over the holidays.
In their annual round-up of the more bizarre fad diets for 2019, the BDA have suggested that the blood type diet, drinking your own pee (yes, really), detox teas/skinny coffee, slimming sachets and alkaline water, are some of the more bizarre regimes they’re coming up against.
Here’s a look at what else is hot in the wellness space, with some links to relevant, recent research that may help you in your daily communications or practice.
Lasting fasting
One thing that has remained popular as we come into the New Year, has been the idea of fasting and this month, Jurassic World actor Chris Pratt, announced to his 22.2 million followers that he’s doing the Daniel Fast.
If you haven’t heard of it, the Daniel Fast was created over a decade ago by Susan Gregory, according to the website, a ‘lay minister, businesswoman, coach for Christian living and wannabe techie’ and is a 21-day period of prayer and partial fasting practised by some Christians, based on the experience of the Prophet Daniel’s and Jewish fasting principles. According to the website, the permitted foods centre around vegan options, with some additional restrictions including all sweeteners (non-nutritive and nutritive), processed foods and solid fats.
Elsewhere and currently number 2 on Amazon.co.uk’s bestseller list for diet books, is Michael Mosley’s ‘The Fast 800’ (in fact it appears twice in the top-10 as a hardback and paperback). His latest offering since the popular 5:2 diet and 8-week Blood Sugar Diet (also still in the top-20), which centres on intermittent fasting/‘time-restricted eating’, is a low-carb, Mediterranean-style diet, based on only 800 calories.
For some recent papers on intermittent fasting in the past year, see the following links:
Flipping the Metabolic Switch: Understanding and Applying the Health Benefits of Fasting
Intermittent Fasting: Is the Wait Worth the Weight?
Compensatory Mechanisms Activated with Intermittent Energy Restriction: a Randomized Control Trial
Intermittent Fasting and Cardiovascular Disease: Current Evidence and Unresolved Questions
Veto keto
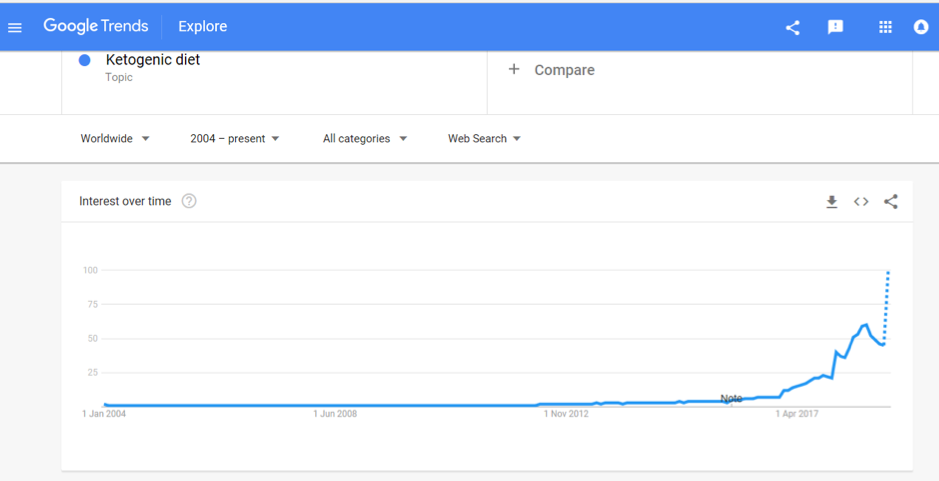
Also vying for the top spot of popular diets in 2019 is the Ketogenic Diet. A quick check of Google search trends shows that after bubbling away for the past few years, interest in this diet is starting to soar and it was the most searched diet term in 2018:

Being low-carb, high fat, the ‘traditional’ Keto Diet may jar against principles of plant-based eating, with new research in The Lancet reaffirming the importance of fibre (from vegetables and wholegrains) in the diet. Keto fans looking for a vegan or vegetarian version of the diet may instead opt for the plant-based version; dubbed ketotarianism, reminiscent of the pegan (paleo-vegan) that was also popular in 2018.
For some helpful papers on ketogenic diets published in the past year, see the following links:
A Nutritional Perspective of Ketogenic Diet in Cancer: A Narrative Review
A Systematic Review of the Use of Ketogenic Diets in Adult Patients with Cancer
The Ketogenic Diet in Disease and Development
Ketogenic Diet for Treatment of Intractable Epilepsy in Adults: A Meta-analysis of Observational Studies
Wellness woo
The Times has also just published an interesting article (which is unfortunately behind a paywall) which to sum up, provides (rather alarming) insight into what’s on the cards for ‘wellness revolutionaries’ in 2019; citing pink coconut water, quartz crystals, salt lamps, MCT oil, edible coffee bars and tongue-scraping, amongst other endeavours, all seemingly in the pursuit of health.
On the other hand, continuing to get good traction is the interest in digestive health and the microbiome, and plant-based eating, with Pinterest’s list of 100 emerging trends for 2019, reporting that searches for oat milk increased in popularity by 186% last year.
It is probably unfair to drop all these increasingly popular approaches into a fad bucket. Some, such as intermittent fasting, have a promising and growing evidence to their name and others may have snippets of beneficial principles in them, such as being plant-based, Mediterranean-style eating or with a focus on minimally processed foods.
Others, however, lack any credibly with regards to the claims they are making; often having inflated what is otherwise an incomplete evidence-base or simply just making things up.
In this era of ‘nutrition folk wisdom’, now more than ever is expertise needed from qualified dietitians and nutrition professionals to make sense of what is becoming an increasingly confusing dietary minefield.
Are there other trends that other dietitians or registered nutritionists do find helpful? Do let us know your thoughts. Or if you are a company and an organisation planning what trends you should support we are always happy to discuss and advise. Call us for a hello on 020 8455 2126 or email hello@nutrilicious.co.uk

by Tanya HAFFNER | Jan 11, 2019 | The Nation’s Health
Happy New Year from the team here at Nutrilicious!
We thought that with the new year comes a great opportunity to take stock and consider what’s lined up for food, nutrition and public health in 2019.
Brexit: Politics and our plates
By far and away, the biggest thing in our diaries for 2019 will be Brexit and what will inevitably mark a fundamental change to the British food system as we’ve come to know it. Come 29 March, the deal will be done (or not!) and what that will look like is anybody’s guess right now.
The UK does not feed itself. We rely heavily on other countries for our food supply, with only 49 per cent of the food consumed in the UK produced here and 30 per cent coming from the EU; the equivalent to 10,000 shipping containers each day. For some commodities such as fruits and vegetables, our dependence on imports is much higher, in this case, we import 90 per cent of the fruits and vegetables we consume.
And so, because our food system is complexly intertwined with the EU, once we leave, it will significantly change our trading relationships, both with the EU, as well as those countries out of the EU that have trading agreements with it.
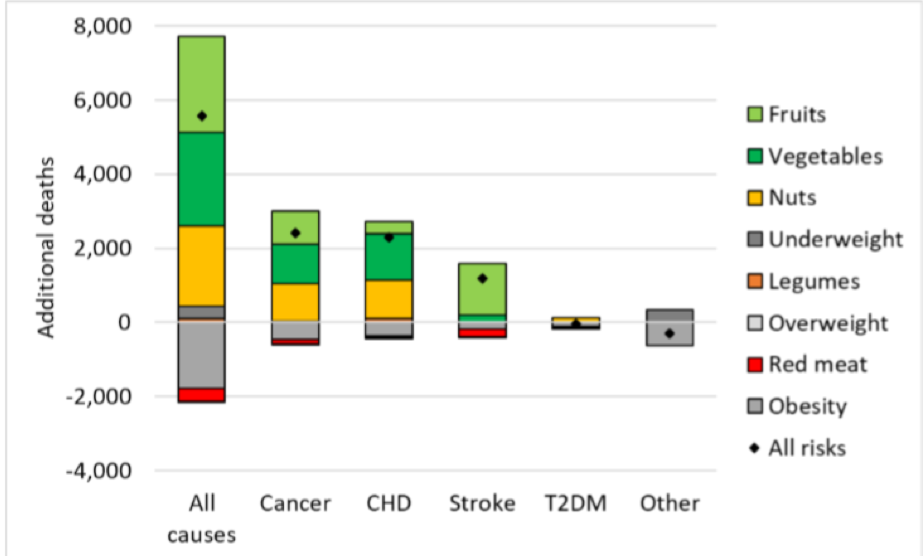
Consequently, people’s diets will be most likely be affected, with a working paper from the Oxford Martin School on the Future of Food warning that food prices are likely to increase, particularly for fruit and vegetables. According to this modelling, a Hard Brexit (trading on World Trade Organisation terms which imposes tariffs on imports) could lead to 5,600 additional deaths per year, associated with reduced consumption of fruits, vegetables, and nuts. This will not only affect individuals but the wider costs to society are pegged at increased healthcare expenditure at around 600 million GBP. On a positive note, there may be small benefits on obesity rates and reduced red meat consumption (see Figure 1)!

Figure 1. Changes in mortality in the UK by risk factor and cause of deaths under a Hard Brexit
The current deal on the table, due to be voted on in mid-January aims to provide a continuous tariff-free and quota-free access to EU markets, but even if voted through, the road ahead is likely to be tumultuous. Initially, the EU Withdrawal Act writes EU law over into UK law – triggering some necessary changes in relation to country of origin labelling and address information. Further changes to our food and nutrition labelling and food regulations may be unavoidable if international trade deals require them.
We should all be watching closely to how Brexit translates to the food on our table, dietary choices and ultimately public health.
For further information on how Brexit may affect the food system, we recommend reading the FRC’s Brexit briefing papers: https://foodresearch.org.uk/food-brexit-briefings/
EAT-Lancet Commission report
We’re expecting that the EAT-Lancet Commission report on Food, Planet, Health, due to launch on 17 January, is going to make waves. Never has the connection between food, planetary and human health been more apparent, with the need to address issues and impacts ever more pressing.
Housed at the Stockholm Resilience Centre, the EAT-Lancet Commission partnership brings together leading global researchers into five working groups, investigating:
- What is a healthy diet?
- What is a sustainable food system?
- What are the trends shaping diets today?
- Can we achieve healthy diets from sustainable food systems? How?
- What are the solutions and policies we can apply?
The report will include the latest research on each of these workstreams and will be publishing targets that deliver for both people and the planet.
For further information and to sign-up for updates, go to the Food, Planet, Health website: https://foodplanethealth.org
If you want to understand more about sustainable diets and how these new targets apply to your business, or would like a scientific review completed on another hot topic, please get in touch on 020 8455 2126.
Coming down the line from government
It looks like the team at Public Health England have been busy. While the rest of us were enjoying our mince pies, they have been working hard behind the sciences and they have kicked off the new year with the launch of new Change4Life messaging, raising awareness of the fact that on average, children are consuming their childhood sugar requirements by 10-years old.
But what else is on the agenda for the year ahead? With the updated Childhood Obesity Strategy published mid-2018 came promises of consultations on bans on pricing and positional promotions in retailers and a 9pm watershed for advertising of unhealthy food and drinks. Though we did see consultations conducted on the ban of sale of energy drinks to children and mandating calorie labelling in the out-of-home sector, some of the other consultations have not materialised yet, but they will be coming this year.
North of the border, the Scottish government also just completed their consultation on restricting junk food promotions, so it will be interesting to see what emerges there.
In 2018, SACN also consulted on their draft review of saturated fats, which recommended a continuation of previous COMA recommendations of 10% total calories. The final report is due at some point 2019 and is on the agenda for discussion at the next SACN meeting in March.
With saturated fat such a hot topic and matter of debate, keep your eyes peeled for this one, as it will provide some much-needed clarity and authoritative recommendations.
In addition, according to SACN meeting notes, the following items should also be expected in 2019:
- Whole Systems Obesity Programme: a joint initiative of PHE, the Local Government Association and the Association of Directors of Public Health are due to publish their guide and tools in the spring
- Product ranges targeted at babies and young children: scope and ambition for this programme is due mid-2019, following initial scoping and consultation that has already been conducted with industry and other stakeholders
- School Food Standards: technical update to commence in 2019
- National Diet and Nutrition Survey Year 1-9 Report: due imminently
So, that’s a brief flavour of some of the key things coming up on 2019. As ever, there’s lots of things to keep us busy!
Here at Nutrilicious we can help with your nutrition and health strategy, nutritional assessments of product portfolios, insights – views from the outside world of nutrition influencers and what they think of your offering – overall helping to put you on the front foot of your competition and upcoming government reformulation targets or standards. Or, perhaps you have key messages that you’d like to share with stakeholders through engaging new media such as interactive webinars and podcasts. To discuss your policy and communication requirements, you can reach us on 020 8455 2126.
Best wishes for a healthy and happy 2019.