
by Nutrilicious | Dec 11, 2015 | Food category comment
The first-meal of the day is changing. Long ago, bacon-and-eggs were popular (and they still are for those anxious about carbohydrates, or for those staying in hotels where others will wash the greasy pans). Then there were periods of battle between toast-and-something or breakfast cereals and milk. Ready-to-eat (RTE) cereals are still the most popular start to the day, but sales are described as, ‘soggy’1 as items that are more portable gain ground: breakfast drinks and biscuits can be orally crammed while running late to the station or school. Or perhaps these on-the-run breakfast products are needed to balance the portable communication bars so constantly held in the other hand?
Other themes have put pressure on manufacturers of RTE cereals. Demands for salt and sugar reduction, demands for gluten-free variants, and shifts in consumer perceptions that carbohydrates are less healthy, and that more proteins is always a good thing.
But most-recent data report that RTE cereals contribute only 8% of free sugars intakes to the diets of children under 10 years of age, and less than 6% to the diets of teenagers2. And what appears extraordinary, is the view of some consumers that the three minutes it may take to eat cereal and milk in the morning, is two minutes too long.
But are these shifts in breakfast patterns a threat to the nutrient quality of diets, which may be a particular issue for the diets of children and teenagers? There is a near-constancy of data supporting the benefits of regularly including nutrient-enriched cereals into diets. Child and adolescent RTE cereal eaters appear be at lower risk of being overweight3,4. Also, breakfast cereal eating is associated with higher intakes of some micronutrients. In a study of more than 1200 European 12-17 year olds4, the RTE cereal-eating teens had higher intakes of various B vitamins, vitamin D, calcium and potassium. A review of various commonly-consumed breakfast cereals5 confirms their contributions to a wide variety of micronutrients, as well a typically contributing to intakes of fibre, whole grain and protein.
Not eating breakfast cereals does not mean not eating these nutrients: there are plenty of other food sources of course. But because they are such a rich and reliable source, it just means that regular intakes are a quick and easy short-cut to the assurance that children and teens have an early-morning head start to better diets. RTE cereal eating may be especially beneficial in the diets of those trying to limit energy6, and in those on low incomes, where there may be a lower variety of other nutrient-dense foods7.
It will be interesting to watch and monitor the national diet and nutrition surveys and see how changing breakfast choices may impact on the nutrient intakes of different groups within the population. In the meantime the slightly unexplained tight-squeeze of time in the morning certainly needs to be battled-against. Some planning of a calm breakfast, the night-before, is one way to encourage the interest of children and teens in sitting down to a few spoons of cereal. The technique of do-as-I-do must also be borne in mind by advocating parents. Lastly, some concessions to variety of products and comforting aura’s helps (suggestion: breakfast Swedish-style with candles and the strict rule of no-electronics at the table!).
Information sources:
- Financial Times Oct 3 2014. Daneshkhu S: Cereal sales go soggy as breakfast shrinks. www.FT.com (accessed 9.11.15)
- Bates B et al (2014) National Diet and Nutrition Survey (NDNS) Result for year 1 to year 4 (combined) of the rolling programme 2008-2012. PHE & FSA, London
- De la Hunty A, Gibson S, Ashwell M (2013) Does regular breakfast cereal consumption help children and adolescents stay slimmer? A systematic review and meta-analysis. Obesity Facts 6, 1, 70-85
- Michels N, De Henauw S, Breidenassel C et al (2015) European adolescent ready-to-eat cereal (RTEC) consumers have a healthier dietary intake and body composition compared to non-RTEC consumers
- Ruxton C (2014) The Role of Breakfast Cereals in Improving Public Health. Complete Nutrition, 14, 3, 69-71
- Reeves S (2015) The Role of Breakfast Cereal in Contributing to Nutrient Shortfalls Associated with Low Calorie Diets. Complete Nutrition, 15, 3, 59-61
- Holmer BA, Kaffa N, Campbell K & Sanders TAB (2012) The contribution of breakfast cereals to the nutritional intake of the materially deprived UK population. European Journal of Clinical Nutrition, 66, 10-17

by Nutrilicious | Dec 11, 2015 | Media in context, The Nation’s Health
The media loves a good headline, and the World Health Organisation (WHO) and the International Agency for Research on Cancer (IARC) provided the perfect story on October 26th – processed meat causes cancer. So is bacon the new tobacco?
The review of over 800 studies found conclusive evidence that processed meats cause colorectal cancer, placing them into the AICR’s top category for carcinogenic substances alongside tobacco. Strong associations were also found for stomach cancer. Red meat was classified as ‘probably causing’ colorectal cancer with the working group unable to exclude all other confounding factors from the data available.
So, are sausages and bacon as bad for us as smoking? Comparing the lowest with the highest consumers, the evidence concluded that for every 50g of processed meat consumed a day, the relative risk of colorectal cancer increased by 18% and for every 100g of red meat consumed daily, the risk increased by 17%.
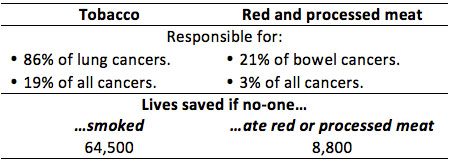
However, when the findings are put into perspective, it is clear that the level of damage caused by smoking is far greater. The IARC, highlights that their findings and risk categories reflect how strong the scientific evidence is for a substance to cause cancer rather than how many incidences of cancer it will actually cause.
Cancer Research UK’s (CRUK) blog on this topic puts things into perspective:
- 61 out of 1,000 people are expected to develop bowel cancer.
- For the lowest meat consumers, this risk will be lower, at around 56 per 1,000.
- For processed meat consumers with a 17% increased relative risk, the incidence would therefore be 66 per 1,000, i.e. 10 more cases per 1,000 for processed vs. non-processed meat consumers.
CRUK went on to put the risk in more real terms.
It’s not about the quality of the meat – it’s all in the cooking or processing technique! The mechanism by which red meat and processed meat cause cancer is still being investigated. However, the current evidence points towards the method of processing and cooking as key drivers for production of carcinogens and there seems little impact with regard to the quality or cut of meat. Processed meats include ancient traditions of smoking, curing and salting as well as any other process to enhance the flavour or shelf life of meat. Included in this category are ham, sausages, bacon, tinned meat and sausages. It is thought that the processing results in the formation of carcinogens within the meat such as N-nitroso-compounds (NOC) and polycyclic aromatic hydrocarbons (PAH).
Get the slow cooker out to help reduce cancer risk! For red meat, which includes pork, beef, lamb and goat, it is the cooking of the meat that seems to generate carcinogenic compounds such as heterocyclic aromatic amines (HAA) and PAH. And these carcinogens like higher temperatures such as those produced during pan frying, grilling and barbecuing.
So how much is too much? On this, there is less clarity as the evidence did not indicate to a ‘safe’ level. CRUK recommends following the current guidelines of no more than 70g red meat per day, avoid processed meat and to use more plant-based protein foods to part or fully replace meat dishes.
How much processed and red meat is the UK currently eating? According to the NDNS data, men eat an average of 86g per day and women 56g. However, there is a significant range from zero for non-meat eaters up to 219g daily for some men. Focusing on the higher processed meat consumers and identifying effective behaviour change strategies seems to be key.
What should our advice be to consumers? Although the Atkin’s supporters may be a little displeased, the average consumer and the press cannot blame scientists and health professionals for always changing their minds. The advice is the same as always…a varied balanced diet, cutting down on red meat and trying to avoid processed meat.
References
- Chan DSM, Lau R, Aune D et al. Red and processed meat and colorectal cancer incidence: meta-analysis of prospective studies. PLoS ONE 6(6): e20456. doi:10.1371/journal.pone.0020456. http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0020456 accessed 5th Nov.
- Bouvard V, Loomis D, Guyton KZ et al. (International Agency for Research on Cancer Monograph Working Group). Carcinogenicity of consumption of red and processed meat. Lancet Oncol. 2015 Oct 23. pii: S1470-2045(15)00444-1. doi: 10.1016/S1470-2045(15)00444-1. [Epub ahead of print] http://www.thelancet.com/journals/lanonc/article/PIIS1470-2045(15)00444-1/abstract Accessed 5th November.
- Dunlop C. Cancer Research UK Science Blog. Processed meat and cancer – what you need to know. 26 October 2015. http://scienceblog.cancerresearchuk.org/2015/10/26/processed-meat-and-cancer-what-you-need-to-know/ Accessed 5th November.

by Nutrilicious | Dec 3, 2015 | Thoughts
This first Sugar Awareness Week, being run by action on sugar, included a reception at the House of Commons yesterday, Wednesday 2nd December, hosted by Geraint Davies MP. The reception was attended by over 100 MPs, NGOs and members of the food industry, all sharing a common interest in sugar reduction, where we were delighted to be invited.
Speeches were made by Geraint Davies MP, the Labour Co-operative Member of Parliament for Swansea West, Dr Alison Tedstone, Director of Diet & Obesity, Public Health England, Tim Smith, Group Quality Director, TESCO, Andrew Opie, Director of Food & Sustainability, British Retail Consortium, and Chairman of Action on Sugar, Professor Graham MacGregor.
Several organisations were in attendance with exhibition stands including the Co-op, Sainsbury’s, Waitrose, Change 4 Life, and Children’s Health Fund amongst others.
The key focus was on the obesity epidemic, the related NHS crisis and action on sugars newly proposed comprehensive approach to preventing obesity and type 2 diabetes in the UK. This has been summarised in their six evidence-based essential actions. This plan has already been submitted to Cameron boldly calling it “Cameron’s plan”. In the words of Professor Graham MacGregor, it is in anticipation that Cameron will have the guts to incorporate it into his forthcoming obesity strategy.
The six evidence-based essential actions:
- Reformulation of sugar and fat in foods and drinks*.
- 50% reduction in sugar content within the next 5 years, starting immediately with sugar-sweetened soft drinks.
- 20% reduction in fat, especially saturated fat, within the next 5 years.
- Stop promotions of unhealthy food & drink*.
- Prevent all types of marketing of unhealthy food and drink to children and adolescents.
- A 20% duty on all sugar-sweetened soft drinks and confectionary, to escalate thereafter if companies do not comply to reformulation targets.
- All public sector food must meet strict guidelines*.
- Uniform colour-coded labelling to be present on all foods for retail and out-of-home, with stricter criteria for high salt, sugars, fat and calories.* (NB sugars as free sugars not total sugars)
* Actions 1, 2, 5 and 6 can only be done by an independent agency e.g. the previous Food Standards Agency or similar. It is action on sugars strong belief that The Department of Health, with the Responsibility Deal, have failed both in its salt and calorie reduction policies. They therefore deem it essential to have an independent (but government-funded) agency who can carry out implementation, thorough monitoring with regulation and enforcement if necessary. Further details on these actions can be found at the web link below.
The adverts highlighted below were developed for this awareness week.




Some key points made by speakers:
Dr Alison Tedstone, Director of Diet & Obesity, Public Health England
- The UK is the first country to recommend no more than 5% of energy as sugar.
- Today, 30% children have tooth decay – we have shameful health stats including obesity which urgently needs to be addressed.
- Part of all this means that sugary drinks should form no part of a children’s diet.
- PHE has carefully analysed the data to determine what action the UK needs to take to reduce sugar intake to come out with their sugar reduction report – evidence for action. While Dr Tedstone highlighted that multiple actions need to be taken she focused on the urgent need to change advertising regulations:
- 40% of the food we buy in the UK is bought on promotion. It’s not neutral. It’s making families buy 1/5th more than they would otherwise buy. It impacts on calorie intake and the balanced diet. Promotions of unhealthy foods should stop.
- Advertising of unhealthy foods in all channels is not neutral. It affects dietary balance and drives towards unhealthy and excessive intakes.
- PHE have advised on the adaptive model with regards to sweeteners recognising that some people will not be able to reduce their likeness for sweet drastically.
Tim Smith, Group Quality Director, TESCO
- TESCOs challenge is to make it easier for the shopper to eat healthier but not compromise on taste.
- Their customers don’t want to be told what to do.
- Small achievable changes are the way to go.
- TESCO has achieved a lot already.
- There are 300,000 employees at TESCO who are taking part in driving healthy eating within.
- They run the Eat Happy Project where 1 million kids have been actively involved.
- The cornerstone has been reformulation.
- 4,000 products over 4 years have been reformulated where the average TESCO customer is consuming 20% less sugar than they were 4 years ago.
- Technical problems are much less than with salt. It’s more about needing the will but we have a business wide commitment on this.
- TESCO are neutral on sugar tax. They will leave it to others to decide.
Andrew Opie, Director of Food and Sustainability, British Retail Consortium
- Retail has achieved a lot already in terms of reformulation. The way has been paved and there continues to be a big focus on sugar alongside fat and salt. There is a lot of experience amongst members.
- We now need reformulation targets to be mandatory. There needs to be a universal adoption. Retailers have led the way in the past and not all in industry have followed. So the bolder companies have sometimes been penalised. This applies critically to key categories that contribute excessively to children’s diets.
Prof Graham MacGregor, Chairman of Action on Sugar
- Action on sugar was set up two years ago and has received a lot of support.
- One year ago they presented a plan to Jeremy Hunt who did nothing.
- This time around Cameron needs to come out with a strong plan to reduce obesity and diabetes.
- Reformulation is key in their recommendations.
- Action on sugar also recommends reducing the sweetness of artificial products to get the population used to less sugar.
- Fat is also highlighted as also important. We need to reduce saturated fat intake and as part of this reduce use of palm oil.
- Action on sugar wants a sugar tax but recognises that in itself, it may not be effective. The income generation and the halo effect however may be important.
In the Q&A session there was some discussion about the call to put teaspoons of sugar on pack. PHE response was that there needed to be more research into how this would be received and utilised. Some suggested that this would purely be for the worried well and therefore not worth the cost.
It was extremely helpful to attend the reception, hear the talks and share experiences with all concerned about sugar intake. It’s been useful to consider action on sugar and public health England’s plans together. We are already incorporating new actions into the various sugar reduction projects that we are involved in. It’s certainly challenging yet very exciting times for both public health and business where creativity and credibility will be key. In the meantime we keenly await “Cameron’s plan” and hopefully in early 2016.
http://www.actiononsugar.org/sugar-awareness-week/Sugar%20Awareness%20Week%202015/167198.html
https://www.gov.uk/government/publications/sugar-reduction-from-evidence-into-action

by Nutrilicious | Nov 11, 2015 | Hot Topics in nutrition, The Nation’s Health
Initial thoughts on the recent PHE Report: Sugar Reduction: The evidence for action
Many realists thought it unthinkable, but it happened, the Scientific Advisory Committee on Nutrition (SACN) recommended that sugar recommendations should be halved. Although many have tried to refute it, the evidence is strong for sugar and dental caries and however anyone tries to pull apart the publications associating sugar intake and weight gain, common sense and practical experience tells us, drinking litres of liquid sugar without any other nutritional benefit is not going to help with our struggle against obesity.
Nevertheless, halving sugar recommendations to no more than 5% of energy intake although aspirational may be a tall ask for many. Some have suggested it unachievable unless applied in a controlled environment where all sugar containing foods are banned. So let’s look at the facts and the plans now in place for achieving this.
Current sugar intakes exceed the old DRV recommendations of no more than 10% energy. Adults were not far off at 11.5%, the issue was with young children and teens with intakes of 14.7% and 15.4% of energy intake respectively. With the new guidelines, we are expecting adults to be able to reduce their sugar intakes by over half and children and teens by three-quarters…that does seem like a tall ask.
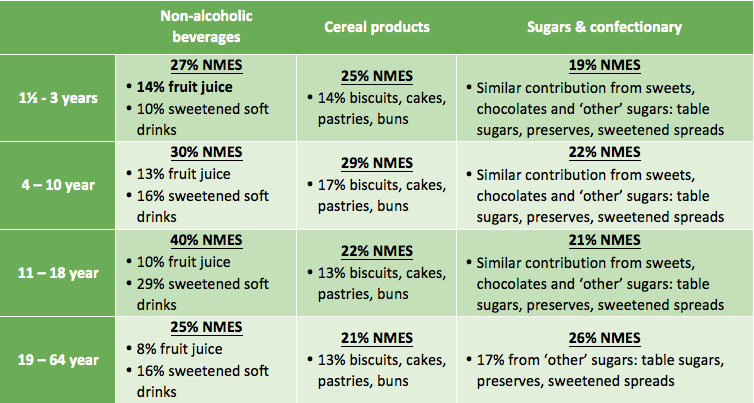
Which are the main culprits?
Food contribution to Non-Milk Extrinsic Sugar (NMES) intakes

Source: National Diet and Nutrition Survey Results from Years 1, 2, 3 and 4 (combined) of the Rolling Programme (2008/2009 – 2011/2012)
Not surprisingly soft drinks are the major contributors to sugar. Other unsurprising contributors are biscuits, cakes, pastries, buns plus obvious sugar and confectionary sources. Surprisingly however, fruit juice is also a key contributor, particularly for the very young. Some health professionals in the past have criticised attacks on fruit juice as it can help contribute to the nation’s 5-a-day. Fruit juice does have a halo effect for contributing to the UK’s vitamin intakes. According to the latest NDNS data, fruit juice contributes towards 14-19% of vitamin C intakes for 4-18 year olds and 12% for adults. However, soft drinks such as energy drinks, cordials and fruit drinks, contribute similar amounts of vitamin C – 18-20%. Whole fruit and vegetables remain top vitamin C contributors. Apart from the vitamin C contribution, fruit juice is not a significant contributor of any other vitamins or minerals, nor is it a source of fibre – a common myth (smoothies would on the other hand contribute to fibre intake). In addition, it’s interesting to note that vitamin C in bought fruit juice is due to fortification and not naturally derived from the fruit source. Based on these facts, soft drinks and fruit juice are not dissimilar, in that they are both a liquid form of concentrated sugar and contribute up to a fifth of vitamin C intakes.
PHE report on a rapid review of the evidence to assess the relationship between fruit juice consumption and health including cardiovascular disease. It reports that the very limited evidence shows no benefit or no harm. However, shouldn’t a review now consider the nutritional composition of fruit juice and its contribution to nutrient intake? This doesn’t appear to have been included. PHE report on how advice has been strengthened to limit consumption of fruit juice to no more than one portion a day i.e. 150ml. However, if 150ml of fruit juice is adhered to, which is highly unlikely given that only 1% of the population currently meet healthy eating guidelines, this in itself will provide approx. three teaspoons of sugar, making up 60% of the recommended maximum free sugars for 4-6 years and 50% in those 7-10 years. A more detailed review of advice in relation to fruit juice seems warranted, particularly in relation to children’s diets.
How can the nation so drastically lower their sugar intakes?
How the government aims to achieve this is through 8 key strategies, published by the PHE on the 22nd October 2015:
- Reduce price promotions on high sugar drinks and foods (in all retail and out of home sections including supermarkets, convenience stores, restaurants, cafes and takeaways).
- Significantly reduce opportunities to market and advertise high sugar food and drink products to children and adults across all media including digital platforms and through sponsorship.
- Set a clear definition for high sugar foods to aid with actions 1 and 2 above. They aim to review and update the 2011 Ofcom nutrient profiling model5.
- Gradual sugar reduction in everyday food and drink products, combined with reductions in portion size.
- The sugar tax. A price increase of a minimum of 10-20% on high sugar products through the use of a tax or levy such as on full sugar soft drinks.
- Government buying standards for food and catering services (GBSF) across the public sector, including national and local government and the NHS to ensure provision and sale of healthier food and drinks in hospitals, leisure centres etc.
- Accredited training in diet and health for all who have opportunity to influence food choices in the catering, fitness and leisure sectors and others within local authorities.
- Continue to raise awareness of sugar to the public as well as health professionals, employers, the food industry etc., encourage action to reduce intakes and provide practical steps to help people lower their own and their families’ sugar intake.
Much of the above makes sense and we look forward to seeing how all of this will be actioned. It comes as no surprise that no single action will be effective in reducing sugar intakes and it’s positive to see much direction for change in terms of the environmental drivers of poor diets. In the meantime we have a number of initial thoughts.
PHE in their report highlight the lack of evidence for a sugar tax where many experts do not support this as an effective strategy. Food tax has failed in some countries where there is limited data for success in others. Placing a 10-20% tax on a cheap commodity such as soft drinks, would surely have little impact on sales where many individuals will simply seek out cheaper own brand alternatives.
While we don’t believe a sugar tax in itself will change sugar intake, any revenue generated from the tax could be put into other actions on reducing sugar intake. However, the halo effect from the extensive media headlines on sugar tax may have in itself already started to impact on inspiring lower sugar food choices. We all know the impact of “celebrity”. However the end impact is rarely positive when it comes to celebrity and public health nutrition. It’s not surprising that Jamie Oliver is once more being regarded as a public health nutrition “angel”.
Banning advertising of sweetened foods and drinks should have come in a long time ago. We know how powerful this tool is, especially for confusing the public with ‘skewed’ health and nutrition claims that seem to by-pass current legislation.
What’s missing?
What could be lacking from the government’s 8-point strategy, is the inclusion of more ‘enforced nudging strategies’ in all retail and out-of-home outlets selling sugary drinks and foods at point of purchase and in areas where there is the highest consumption. Removing high sugar foods and drinks from end of aisles and till points are mentioned. However, very little weight is given to this in the summary, despite that fact that this strategy has been proven to work in many scenarios both in the UK and abroad. Many corner shops and out-of-home food establishments have a limited range of ‘sugar free’ drink variants, bottled water is often highly priced, and point of purchase is often adorned with high sugar / fat /salt snacks and in some well-known establishments, 500g chocolate bars are aggressively promoted.
Another dichotomy is the drive for industry sugar reductions within major sugar contributors such as confectionary, cakes, biscuits and sweetened drinks. While this is needed as an immediate and realistic solution (changing peoples’ behaviour and eating habits will take a number of generations!), on its own, it cannot help towards improving the overall dietary and lifestyle habits of individuals. Swapping like with like will not educate or help change behaviour to enjoy and consume sugar / high fat foods in moderation nor can it empower the most in need to increase fruit and vegetable, water, wholegrains, oil-rich fish and plant-based protein intakes and be more physically active. This is an important factor that needs to be incorporated into any responsible reformulation programme and subsequent communication plans.
There are of course a number of challenges associated with removing sugar from a food or drink product and there little mention of this in the report. Positively industry have already been reformulating and achieving significant reductions in the sugar content of foods and drinks already, particularly in relation to retail own brands. A range of solutions have been employed which include the use of high intensity sweeteners, some bulking agents alongside some fibres. Adding fibre successfully provides a big opportunity for businesses and public health where the population are not eating enough fibre and where SACN has recently recommended increases in daily intakes. These of course all come with various challenges which need to be considered in full before embarking on re-formulation. The use of sweeteners for example are tightly regulated at EU level. There are restrictions for use on some sweeteners in some food groups. Claims in relation to sugar reduction are also tightly regulated. Importantly the other challenge is to reformulate in ways that still deliver on the consumer expectation for taste. A challenge for all industry members and particularly medium and start-up companies of course will be cost of re-formulation.
Competent training in diet and health for the wider workforce has been hugely welcomed at Nutrilicious. This is a key passion and area of work for us. The power of many occupations and individuals to influence the diet and health of those they have contact with is enormous. Yet many lack training. Guidance on how to achieve this is mentioned but one of the key stumbling blocks for most which is funding is not addressed in this report.
Something we feel PHE failed to tackle, possibly due to the enormity of the task, is food labelling. Regulations and guidance for front and back of pack labelling stipulates that ‘Total’ sugar must be shown. There are justifiable technical reasons for this. With the increase of front of pack traffic light labelling and encouragement of its use by the government, this is bound to thwart any attempts by individuals to fully grasp which sugars they should be avoiding and more importantly, the importance of nutrient dense foods. Focusing on just sugar content on food labels, the consumer could not be blamed for choosing digestive biscuits over an individual portion of nuts and raisins. The former would be traffic light coded amber for sugar and display 17.5g sugar per 100g (or 4.6g per 2 biscuits) whilst a 25g nuts and raisins pack would be traffic light coded red for sugar and display 34g sugar per 100g (8.5g per serve). How are we helping the consumer understand that the latter will not contribute to ‘free sugars’ and more importantly, it would help towards meeting the new increased fibre recommendations, provide heart healthy fats and some minerals. How confusing can it be for a consumer to see plain dairy yogurt with amber traffic light for sugar at 7.5g per 100g. Is there now a real need for the UK to adopt front of pack traffic light labelling for sugar to only include added sugar?
Focusing more on positive messages about foods rather than individual nutrients must be a major part of the way forward. And to drive positive food choices, it would be paramount to make naturally healthier foods more attractive and readily available whilst reducing the shelf space in stores of highly processed high sugar and fat foods with little other nutritive value.
Driving healthy food choices involves nudging people in the right direction as well as helping them to learn how to achieve a healthy balanced relationship with all foods and drinks (not nutrients). All stakeholders across multiple sectors and channels can play their own unique role in this and its exciting times for those developing and creating new food and health strategies and engagement plans for better health and business.
While lots of thoughts questions and ideas abound, we welcome PHEs report on sugar reduction. We look forward to working with relevant partners in contributing to the action and seeing how all of this will be implemented and monitored so that the 5% target can be achieved in 10 years.
At this date PHE have kindly agreed for us to interview them in January 2016 about this report and we look forward to exploring our thoughts and questions further on this hot public health strategy.
https://www.gov.uk/government/publications/sugar-reduction-from-evidence-into-action

by Nutrilicious | Nov 9, 2015 | Changing mindset
Mindfulness is often used to promote well being and help reduce stress and anxiety and considerable benefits have been shown from a large body of research in positive psychology. In essence mindfulness practice teaches us to pay full attention in the present moment, non judgementally to our physical and emotional experiences. 1
Several studies have looked at the potential benefits of applying these techniques to eating. Researchers point out that of the multiple daily decisions we make about food, most are unconscious often resulting in overeating and other unhealthy eating patterns. Mindful eating aims to raise our awareness of the internal and external environments before, during and after eating and the reasons behind some of our decisions we make with the aim of improving diet. As shown in Figure 1 mindful eating may explore the “why, what, when and where” of our food consumption as well as the “how”( including speed of eating) and “how much” (portion size).
Figure 1 The Mindful Eating Cycle

Mindful eating aims to promote awareness not only of the nutritional content of our food but other qualities such as the appearance, smell, taste and texture. It may focus attention on the environmental triggers to overeating, the thoughts and feelings that arise when we eat, how we deal with guilt or anxiety around food and the role of unhelpful distractions like TV or social media in causing overeating.
Several studies show that speed of eating is associated with higher energy intakes and greater risk of obesity. 2-3 In addition eating as a genuine response to hunger and satiety signals (intuitive eating) is strongly associated with a lower body mass index 4. Mindfully slowing eating and allowing a delay for satiety to register, may therefore be an effective strategy to help prevent or manage obesity.
Mindless consumption of large portion sizes of food and drink are also strongly linked with higher energy consumption and risk of obesity. 5 Some studies show those who score highest on measures of mindful eating, in particular those who pay attention to their emotions and feelings around eating, eat smaller portions of energy dense foods. 6 Even brief teaching of mindful eating techniques have been shown to reduce overeating on unhealthy snacks (such as chocolate chip cookies in one study) when we are particularly hungry. 7
In a recent review of 61 studies, researchers consistently found the larger the amount of food we serve ourselves the more is eaten . 8 Mindfully reducing triggers to overeating such as large portions and tableware sizes, repackaging or purchasing single portion package sizes and placing unhealthy foods or leftovers out of sight may be effective behaviour tools to moderate the types or quantities of food consumed.
Mindful eating strategies can help promote evidence based behaviour change commonly advised for improving health as recommended in public health interventions.
For example some of the effective eating behaviour strategies to help weight loss which may be promoted by mindful eating techniques are shown in shown in Table 1.
Table 1 Some evidence based eating behaviour strategies advised to help weight loss which can be promoted by mindful eating techniques
 Adapted in part from NDR- UK 9402 Changing For Good 11
Adapted in part from NDR- UK 9402 Changing For Good 11
In addition to a role in weight management, mindful eating has been shown to help people improve diet in a wide range of conditions including eating disorders, metabolic syndrome and diabetes. 9-10 Regular practice may also increase awareness of the positive and nurturing opportunities of food preparation and consumption.
To be successful mindful eating needs to learnt and developed by regular and confident practice. For instance studies show that people who make permanent changes to eating patterns are more likely to lose weight and keep it off.
At present there are few large, randomised studies on mindful eating and further research would be useful. However, mindfulness techniques which can be taught may be a useful and effective addition to the toolbox for improving informed, conscious choices around eating which could include any food behaviour change strategy or related communication programme.
References
1. Ludwig DS and Kabat-Zinn J (2008) Mindfulness in medicine. JAMA. 300 : 1350-2
http://www.ncbi.nlm.nih.gov/pubmed/18799450 (Accessed November 2015).
2. Leong SL ,Madden C, Gray A et al ( 2011) Faster self reported speed of eating is related to higher body mass index in a nationwide survey of middle –aged women. J Am Diet Assoc 111: 1192-7
http://www.ncbi.nlm.nih.gov/pubmed/21802566 (Accessed November 2015).
3. Otsuka R, Tamakoshi, K Yatsuya H et al (2006) Eating fast leads to obesity: findings based on self-administered questionnaires among middle-aged Japanese men and women.
http://www.ncbi.nlm.nih.gov/pubmed/16710080 (Accessed November 2015).
4. Madden CE, Leong SL, Gray A et al ( 2012) Eating in response to hunger and satiety signals is reacted to BMI in a nationwide sample of 1601 mid – age New Zealand women. Public Health Nutr 15 : 2272-9 http://www.ncbi.nlm.nih.gov/pubmed/22443858 (Accessed November 2015)
5. Wansink B (2011) B Mindless Eating : why we eat more than we think. Hay House UK. http://mindlesseating.org/ (Accessed November 2015).
6. Beshara M, Hutchinson AD and Wilson C ( 2013) Does mindfulness matter? Everyday mindfulness, mindful eating and self-reported serving size of energy dense foods among a sample of South Australian adults. Appetite 67: 25-9
http://www.ncbi.nlm.nih.gov/pubmed/23548262 (Accessed November 2015).
7. Marchiori D and Papies EF ( 2014) A brief mindfulness intervention reduces unhealthy eating when hungry, but not the portion size effect. Appetite 75: 40-5
http://www.ncbi.nlm.nih.gov/pubmed/24361312 (Accessed November 2015).
8. Hollands GJ, Shermilt, I Marteau TM et al (2015) Portion, package or tableware size for changing selection and consumption of food, alcohol and tobacco. Cochrane Library September 2015.
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD011045.pub2/abstract.
(Accessed November 2015).
9. Kristeller JL, Wolever RQ (2011) Mindfulness-based eating awareness training for treating binge eating disorder: the conceptual foundation. Eating Disorders 19:49-61.
10. Miller CK, Kristeller JL, Headings A et al.(2012) Comparative effectiveness of a mindful eating intervention to a diabetes self-management intervention among adults with type 2 diabetes: a pilot study. J Acad Nutr Diet. 112:1835-1842.
11. Changing for good NDR- UK Ref 9402
http://www.ndr-uk.org/vmchk/Weight-management/Changing-for-Good.html (Accessed November 2015).







 Adapted in part from NDR- UK 9402 Changing For Good 11
Adapted in part from NDR- UK 9402 Changing For Good 11