by Suellen Morris | Apr 27, 2023 | Hot Topics in nutrition, Thoughts, The Nation’s Health, Education
This month, we are pleased to see the publication of a paper that Nutrilicious were commissioned to create. While our nutrition and science team at Nutrilicious strongly believes that we must now update the Eatwell Guide we also believe that more focus must be given to communications of the Eatwell Guide. The new rapid review explores communications around food based dietary guidelines (FBDG), including the Eatwell Guide. The paper has been published in the journal ‘sustainability’ , authored by Amy E Culliford, Jane Bradbury and Elphee B. Medici. As a nutrition and sustainable diets communications consultant at Nutrilicious, Elphee was part of the core research team for this project.
Improving Communication of the UK Sustainable Healthy Dietary Guidelines the Eatwell Guide: A Rapid Review

Background
In the UK, FBDG are reflected by the Eatwell Guide, developed by Public Health England (PHE), last updated in 2016. The Eatwell Guide replaced the Eatwell Plate and continues to define the government’s advice on a healthy balanced diet. The visual guide provides a representation of healthy eating by splitting the food we eat into five food groups and shows how much an individual should eat from each group. The supporting guides that can be found on the government’s website include A colour Eatwell Guide PDF, Government dietary recommendations, The Eatwell Guide Booklet and A quick guide to the government’s healthy eating recommendations

Currently, only 0.1% of the UK population are meeting all nine recommendations provided by the Eatwell Guide. Improving adherence is of upmost importance not only to improving health and reducing rates of non-communicable disease in the UK but also to supporting a reduction in the environmental impact of what we are eating, to help meet the UK’s targets in reducing greenhouse gas emissions (GHGe) by 68% by 2023, compared to 1990 levels.
The Findings
Key themes were pulled out as part of the review as being significant in effective communication of FBDG. The following five recommendations were made, with the aim of helping to improve adherence to the Eatwell Guide:
(1) Review of language and tone of nutrition and sustainability related messages
Short, simple, specific and easy to understand communications should be utilised, using an empathetic and empowering tone. Specific messages relating to sustainable diets should be recommended and incorporated into guidelines offering benefits for the people and the planet.
(2) Targeting of FBDG and communications to specific population segments
Communication needs to be tailored and appeal to different population groups including age, gender, cultural background and motivation style. Further research is warranted to explore factors which influence food choices within specific target population segments.
(3) Addressing barriers to and benefits of adopting the Eatwell Guide recommendations
Barriers need to be addressed to guide in effective communications. Barriers identified included taste preferences, cost, time and habits.
(4) Development of practical tools and resources to support implementation of the guidelines
Compared to other countries’ FBDG communication strategies, the UK is currently lacking in producing supporting resources to assist in the implementation of the Eatwell Guide. For example, portion size guidance for various population groups, healthier and tasty substitutions for unhealthy and/or unsustainable foods would be beneficial and also recipes and practical approaches to meeting FBDG.
(5) Leveraging social media and social marketing techniques to increase public engagement
Social media and the internet are a key target area to communicate to individuals. The digital space should be utilised to form a key part of the Eatwell Guide communication strategy, alongside traditional media.
As can be seen, multiple elements need to be considered when communicating the Eatwell Guide to the public, health professionals and other stakeholders.
Moving On
The review provides such valuable lessons into the effective use of FBDG, including what has been working well globally. Research findings from this new rapid review can help to drive better and more effective communication strategies in order to promote sustainable healthy eating guidelines. Policy makers, the food industry and health professionals should use this to drive dietary behaviour change. The authors conclude that further research is needed in this area, with a particular focus on ‘research into the motivations, perceived barriers and preferred communication style for target population groups and a more detailed analysis of social marketing and industry strategies which could be adapted to promote sustainable healthy diets.’
“Healthy eating guidance including the Eatwell Guide need to be brought to life through a strategic and creative marketing strategy designed to resonate with different population groups and on a level similar to how food marketing is successfully done. Government needs to go beyond current guidelines and campaigns and embed this into an always-on public health strategy to make this happen. Those involved in such a strategy would benefit from the learnings in this paper” – Tanya Haffner, Registered Dietitian, CEO Nutrilicious

by Nutrilicious | Sep 20, 2019 | Thoughts, The Nation’s Health, Education
When it comes to food choices, what should we be advising those suffering from type 2 diabetes to help them manage weight and glucose?
Do we focus on a low carb diet?
Cutting out fat?
Or just the simple principle of sticking to Eatwell guidelines?
Media headlines continue to offer 101 different – conflicting – solutions. So what’s the truth? How can we piece together this apparent mess to best support those with diabetes?
Next week, in the second in our series of diabetes NutriWebinars, expert Dr Duane Mellor, RD, Senior Teaching Fellow at Aston Medical School, Aston University will be exploring these topics.
Looking at how advice has shifted over the past few decades, he’ll be talking through the latest evidence and explaining what health professionals can do to actually help people living with type 2 diabetes.
The webinar will also cover evidence from the last couple of years that shows that type 2 diabetes is not necessarily always a condition for life: through weight loss and maintenance, we can actually help people go into remission.
Fundamentally, it’s about putting the person with the condition at the centre – rather than trying to force them into eating habits that don’t suit their lifestyle, culture or preferences. Instead of concentrating on specific nutrients at specific times of the day – ‘you must have starchy carbs at breakfast’ – it’s working out what works for them, at the same time as creating an overall balanced diet.
Inviting questions and ideas from participants, the NutriWebinar is set to be an interesting, informative and empowering evening. (Plus, it’s free and counts as CPD.) We hope you’ll join us and encourage colleagues to join in too: register now

by Nutrilicious | Jun 14, 2019 | The Nation’s Health
‘The levy is working.’ That’s the conclusion from a recent survey of drinks sales, a year on since the Soft Drinks Industry Levy (SDIL) – or sugar tax – was introduced.
The study concentrated on products that sell in large enough volume to have a public health effect. In a ‘historic change’, sales of Coke Zero Sugar increased by 50 per cent and Pepsi, sugar-free Max by 17 per cent. Full sugar Classic Coke and Blue Pepsi sales both fell.
The shift is attributed to the sugar free drinks being cheaper than their full sugar equivalent, as a result of the SDIL. Giving consumers the economic incentive to buy drinks that are healthier has worked. As the authors of the study say, ‘Discounts have had the effect that economists expected and health specialists hoped for.’
New sugar free versions of popular drinks are being increasingly sold in major retailers, with the hope that they’ll also become more prominent in smaller, independent shops. The positive trend is moving in the right direction – and it’s happening relatively quickly.
More needs to be done from a retail environment point of view, especially alerting customers to the discounts. Non-lead brands do still have work to do on reducing their sugar levels – although affecting a far smaller number of individuals, they still impact on health. And of course, the drinks industry is just one part of the wider obesity story.
We wondered what the effect of the sugar tax would be when it was introduced. So it’s fantastic to hear the dramatic change that’s already happened – and we’ll be monitoring the year ahead with interest.
The study was carried out by Jack Winkler, Emeritus Professor of Nutrition Policy, London Metropolitan University and Tam Fry, chair National Obesity Forum. Go to BeverageDaily.com to read the full results

by Nutrilicious | Apr 16, 2019 | The Nation’s Health, Changing mindset, Impactful health initiatives
We’re excited to be involved in a new initiative to help tackle the critical problem of poor diet amongst lower income households: Shop Well – Eat Well. It’s a collaboration between the British Dietetic Association (BDA), Alpro and the Southwark Hub, with the aim of a multi-angled approach to have a real and lasting impact.
Launched last month, we brought together experts to give their insights into key topics. Here’s a summary of some of the key points, followed by links to each of the presentations, which we highly recommend you take the time to watch!
People on lower incomes have a worse diet and shorter life expectancy
There is a direct correlation between diet and income, in turn affecting health. The lower your income, the more likely it is you will:
- Eat more sugar, processed foods, fat and sodium
- Eat less fibre, vitamin A and folate
- Be less likely to meet iron, folate and calcium recommendations
- Eat less oil-rich fish
- Eat more take-aways
- Cook less at home from scratch
People in lower income groups in the UK have a significantly shorter life expectancy than the average: by nine years for women and seven for men.
They have double the rates of cardiovascular disease, lifestyle-related cancers, type 2 diabetes and total mortality compared to the national average. Obesity prevalence of the most deprived 10% of children is approximately twice that of the least deprived 10%.
This is not new news. Countless attempts have been made to try to address the problem and encourage people on lower incomes to eat more healthily, thereby increasing their quality of life and life expectancy.
But when it comes to eating habits, behaviour change is very difficult to achieve.
Barriers to healthy eating are multiple, complex and interlinked – psychological, financial, environmental, conscious and unconscious. Among lower income households they include:
- Financial barriers – For low income families, a big barrier to buying new foods or going to a new food shop is not knowing how much the food will cost, or assuming that it will all be expensive. Parents want to know exactly how much their shopping basket is before they reach the checkout.
- Social barriers – Food habits get passed down the generations as young people grow up and become parents themselves. What children see their parents and families doing is what they grow up thinking of as ‘normal’.
- Preparation space – Cooking from scratch relies on kitchen equipment, confidence in cooking skills, time to prepare food and pleasant surroundings – not the case for many on low income.
- Limited bandwidth – The cognitive burden of living under financial strain and other modern day life stresses reduce parents‘ mental bandwidth; brainpower that would otherwise go to planning ahead and problem-solving.[1] Families in this situation look for quick and easy ways to eat, and takeaway and convenience foods provide an in-the-moment solution to feeding children quickly, affordably and safely.
- Advertising and shop layouts – Cues such as special offers, advertising for takeaways, attractive packaging and child-height shelving nudge families towards less healthy foods in shops.
- It’s not always a lack of knowledge or cost that’s a problem, it’s translating knowledge to practice.
In fact, most eating behaviour is driven by unconscious, habitual processes. These are largely immune to education when it comes to behaviour change. Yet this has been our predominant approach to changing dietary behaviour!
Breaking the habits of a lifetime
Multiple collaborative strategies are needed to succeed in changing behaviour: from government, local authority, industry and all food providers, alongside continuing to help individuals overcome their personal barriers.
We need to making healthy eating
- easy,
- habitual, and
- normal
As behavioural psychologist Dr. Paul Chadwick says, it’s not sustainable for people to have to think about every food choice that they make. Healthy eating has to become the default option.
A new initiative for change
Behavioural science shows the importance of interactions between the individual and their physical and social environment when it comes to habit forming and breaking.
It’s time the food environment changed to make healthy eating as easy to attain as possible for all, including low affluent groups.
It’s also time for families and individuals to be supported in overcoming barriers to breaking the unhealthy habits.
 We’re excited to be part of the new initiative, Shop Well – Eat Well, to help enable this – especially targeting those on a low income.
We’re excited to be part of the new initiative, Shop Well – Eat Well, to help enable this – especially targeting those on a low income.
Starting as a year-long pilot in Southwark, South London, it’s kicking off in June. Community charities and volunteers will join to create peer and professional-led healthy eating seminars and workshops tailored to the young, old and families.
At the launch, Kate Arthur, UK External Scientific Affairs & Nutrition Manager at Alpro, explained: “We wanted to find interventions that would encourage people to think about their food choices differently.
“Going directly into the community to find out what will work for people is the logical thing to do. We’ll be working on different engaging activities such peer led cookery workshops and drop in seminars, with help from the BDA Let’s get Cooking and an advisory committee of experts, always with an eye on the main barriers.
“Ultimately, we’ll be assessing to see what really makes a difference over the next year of the campaign and we’ll share any success stories widely with local communities nationwide and the dietetic community as a whole.”
Caroline Bovey, Chair of the British Dietetic Association added: “By partnering on this project, and working with the food manufacturers and shops that people are accessing daily, we’re excited to directly tackle some of the wider barriers to healthy habits in a local area. The BDA is delighted to be working with Alpro and the Southwark wellbeing hub to help people who often have to prioritise the other demands of daily life over their food choices.”
Take advantage of insightful presentations and useful resources
At our launch, five leading experts presented the latest evidence and initiatives to help overcome barriers to healthy shopping baskets and healthy eating. The presentations are available on the Shop Well – Eat Well website. Make yourself a cup of tea, watch, learn and be inspired:
– Dr Paul Chadwick, behaviour change leading expert: A scientific approach to behaviour change
– Sue Baic, Registered Dietitian: Affordable, healthy and sustainable eating in practice
– Duncan Brown, Development Director at charity Shift design: How does affluence impact on food choices?
– Kate Arthur, Alpro UK’s External Scientific Affairs & Nutrition Manager: Changing behaviour in the community
– Nilani Sritharan, Company Nutritionist at Sainsbury’s Supermarkets Ltd: Making healthy shopping easier
You’ll also find practical and engaging resources to help consumers overcome their barriers to healthy eating.
#shopwelleatwell @SouthwarkHub @BDA_Dietitians @Alpro

by Tanya HAFFNER | Jan 17, 2019 | Hot Topics in nutrition, The Nation’s Health
What’s hot in the wacky world of wellness in 2019
Historians believe that the practice of New Year resolutions originated in the Babylonian Kingdom, over 3,000 years ago. New Year intuitively brings time for pause, reflection and setting intentions for the year, and for many, that can centre on resetting what they eat, especially after indulging over the holidays.
In their annual round-up of the more bizarre fad diets for 2019, the BDA have suggested that the blood type diet, drinking your own pee (yes, really), detox teas/skinny coffee, slimming sachets and alkaline water, are some of the more bizarre regimes they’re coming up against.
Here’s a look at what else is hot in the wellness space, with some links to relevant, recent research that may help you in your daily communications or practice.
Lasting fasting
One thing that has remained popular as we come into the New Year, has been the idea of fasting and this month, Jurassic World actor Chris Pratt, announced to his 22.2 million followers that he’s doing the Daniel Fast.
If you haven’t heard of it, the Daniel Fast was created over a decade ago by Susan Gregory, according to the website, a ‘lay minister, businesswoman, coach for Christian living and wannabe techie’ and is a 21-day period of prayer and partial fasting practised by some Christians, based on the experience of the Prophet Daniel’s and Jewish fasting principles. According to the website, the permitted foods centre around vegan options, with some additional restrictions including all sweeteners (non-nutritive and nutritive), processed foods and solid fats.
Elsewhere and currently number 2 on Amazon.co.uk’s bestseller list for diet books, is Michael Mosley’s ‘The Fast 800’ (in fact it appears twice in the top-10 as a hardback and paperback). His latest offering since the popular 5:2 diet and 8-week Blood Sugar Diet (also still in the top-20), which centres on intermittent fasting/‘time-restricted eating’, is a low-carb, Mediterranean-style diet, based on only 800 calories.
For some recent papers on intermittent fasting in the past year, see the following links:
Flipping the Metabolic Switch: Understanding and Applying the Health Benefits of Fasting
Intermittent Fasting: Is the Wait Worth the Weight?
Compensatory Mechanisms Activated with Intermittent Energy Restriction: a Randomized Control Trial
Intermittent Fasting and Cardiovascular Disease: Current Evidence and Unresolved Questions
Veto keto
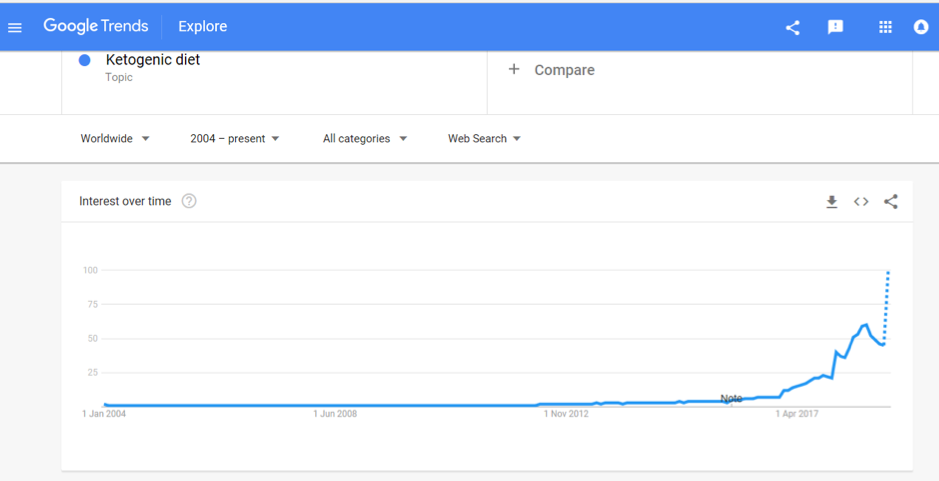
Also vying for the top spot of popular diets in 2019 is the Ketogenic Diet. A quick check of Google search trends shows that after bubbling away for the past few years, interest in this diet is starting to soar and it was the most searched diet term in 2018:

Being low-carb, high fat, the ‘traditional’ Keto Diet may jar against principles of plant-based eating, with new research in The Lancet reaffirming the importance of fibre (from vegetables and wholegrains) in the diet. Keto fans looking for a vegan or vegetarian version of the diet may instead opt for the plant-based version; dubbed ketotarianism, reminiscent of the pegan (paleo-vegan) that was also popular in 2018.
For some helpful papers on ketogenic diets published in the past year, see the following links:
A Nutritional Perspective of Ketogenic Diet in Cancer: A Narrative Review
A Systematic Review of the Use of Ketogenic Diets in Adult Patients with Cancer
The Ketogenic Diet in Disease and Development
Ketogenic Diet for Treatment of Intractable Epilepsy in Adults: A Meta-analysis of Observational Studies
Wellness woo
The Times has also just published an interesting article (which is unfortunately behind a paywall) which to sum up, provides (rather alarming) insight into what’s on the cards for ‘wellness revolutionaries’ in 2019; citing pink coconut water, quartz crystals, salt lamps, MCT oil, edible coffee bars and tongue-scraping, amongst other endeavours, all seemingly in the pursuit of health.
On the other hand, continuing to get good traction is the interest in digestive health and the microbiome, and plant-based eating, with Pinterest’s list of 100 emerging trends for 2019, reporting that searches for oat milk increased in popularity by 186% last year.
It is probably unfair to drop all these increasingly popular approaches into a fad bucket. Some, such as intermittent fasting, have a promising and growing evidence to their name and others may have snippets of beneficial principles in them, such as being plant-based, Mediterranean-style eating or with a focus on minimally processed foods.
Others, however, lack any credibly with regards to the claims they are making; often having inflated what is otherwise an incomplete evidence-base or simply just making things up.
In this era of ‘nutrition folk wisdom’, now more than ever is expertise needed from qualified dietitians and nutrition professionals to make sense of what is becoming an increasingly confusing dietary minefield.
Are there other trends that other dietitians or registered nutritionists do find helpful? Do let us know your thoughts. Or if you are a company and an organisation planning what trends you should support we are always happy to discuss and advise. Call us for a hello on 020 8455 2126 or email hello@nutrilicious.co.uk

by Tanya HAFFNER | Jan 11, 2019 | The Nation’s Health
Happy New Year from the team here at Nutrilicious!
We thought that with the new year comes a great opportunity to take stock and consider what’s lined up for food, nutrition and public health in 2019.
Brexit: Politics and our plates
By far and away, the biggest thing in our diaries for 2019 will be Brexit and what will inevitably mark a fundamental change to the British food system as we’ve come to know it. Come 29 March, the deal will be done (or not!) and what that will look like is anybody’s guess right now.
The UK does not feed itself. We rely heavily on other countries for our food supply, with only 49 per cent of the food consumed in the UK produced here and 30 per cent coming from the EU; the equivalent to 10,000 shipping containers each day. For some commodities such as fruits and vegetables, our dependence on imports is much higher, in this case, we import 90 per cent of the fruits and vegetables we consume.
And so, because our food system is complexly intertwined with the EU, once we leave, it will significantly change our trading relationships, both with the EU, as well as those countries out of the EU that have trading agreements with it.
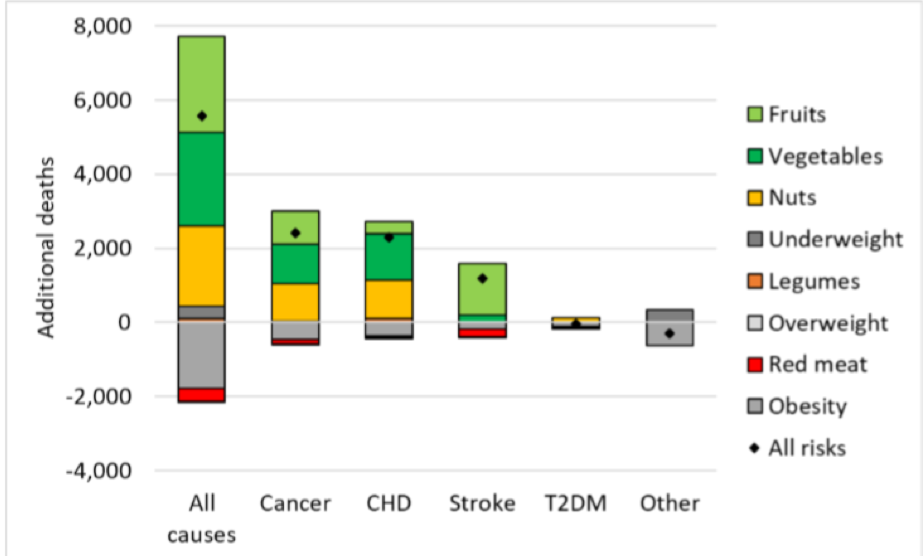
Consequently, people’s diets will be most likely be affected, with a working paper from the Oxford Martin School on the Future of Food warning that food prices are likely to increase, particularly for fruit and vegetables. According to this modelling, a Hard Brexit (trading on World Trade Organisation terms which imposes tariffs on imports) could lead to 5,600 additional deaths per year, associated with reduced consumption of fruits, vegetables, and nuts. This will not only affect individuals but the wider costs to society are pegged at increased healthcare expenditure at around 600 million GBP. On a positive note, there may be small benefits on obesity rates and reduced red meat consumption (see Figure 1)!

Figure 1. Changes in mortality in the UK by risk factor and cause of deaths under a Hard Brexit
The current deal on the table, due to be voted on in mid-January aims to provide a continuous tariff-free and quota-free access to EU markets, but even if voted through, the road ahead is likely to be tumultuous. Initially, the EU Withdrawal Act writes EU law over into UK law – triggering some necessary changes in relation to country of origin labelling and address information. Further changes to our food and nutrition labelling and food regulations may be unavoidable if international trade deals require them.
We should all be watching closely to how Brexit translates to the food on our table, dietary choices and ultimately public health.
For further information on how Brexit may affect the food system, we recommend reading the FRC’s Brexit briefing papers: https://foodresearch.org.uk/food-brexit-briefings/
EAT-Lancet Commission report
We’re expecting that the EAT-Lancet Commission report on Food, Planet, Health, due to launch on 17 January, is going to make waves. Never has the connection between food, planetary and human health been more apparent, with the need to address issues and impacts ever more pressing.
Housed at the Stockholm Resilience Centre, the EAT-Lancet Commission partnership brings together leading global researchers into five working groups, investigating:
- What is a healthy diet?
- What is a sustainable food system?
- What are the trends shaping diets today?
- Can we achieve healthy diets from sustainable food systems? How?
- What are the solutions and policies we can apply?
The report will include the latest research on each of these workstreams and will be publishing targets that deliver for both people and the planet.
For further information and to sign-up for updates, go to the Food, Planet, Health website: https://foodplanethealth.org
If you want to understand more about sustainable diets and how these new targets apply to your business, or would like a scientific review completed on another hot topic, please get in touch on 020 8455 2126.
Coming down the line from government
It looks like the team at Public Health England have been busy. While the rest of us were enjoying our mince pies, they have been working hard behind the sciences and they have kicked off the new year with the launch of new Change4Life messaging, raising awareness of the fact that on average, children are consuming their childhood sugar requirements by 10-years old.
But what else is on the agenda for the year ahead? With the updated Childhood Obesity Strategy published mid-2018 came promises of consultations on bans on pricing and positional promotions in retailers and a 9pm watershed for advertising of unhealthy food and drinks. Though we did see consultations conducted on the ban of sale of energy drinks to children and mandating calorie labelling in the out-of-home sector, some of the other consultations have not materialised yet, but they will be coming this year.
North of the border, the Scottish government also just completed their consultation on restricting junk food promotions, so it will be interesting to see what emerges there.
In 2018, SACN also consulted on their draft review of saturated fats, which recommended a continuation of previous COMA recommendations of 10% total calories. The final report is due at some point 2019 and is on the agenda for discussion at the next SACN meeting in March.
With saturated fat such a hot topic and matter of debate, keep your eyes peeled for this one, as it will provide some much-needed clarity and authoritative recommendations.
In addition, according to SACN meeting notes, the following items should also be expected in 2019:
- Whole Systems Obesity Programme: a joint initiative of PHE, the Local Government Association and the Association of Directors of Public Health are due to publish their guide and tools in the spring
- Product ranges targeted at babies and young children: scope and ambition for this programme is due mid-2019, following initial scoping and consultation that has already been conducted with industry and other stakeholders
- School Food Standards: technical update to commence in 2019
- National Diet and Nutrition Survey Year 1-9 Report: due imminently
So, that’s a brief flavour of some of the key things coming up on 2019. As ever, there’s lots of things to keep us busy!
Here at Nutrilicious we can help with your nutrition and health strategy, nutritional assessments of product portfolios, insights – views from the outside world of nutrition influencers and what they think of your offering – overall helping to put you on the front foot of your competition and upcoming government reformulation targets or standards. Or, perhaps you have key messages that you’d like to share with stakeholders through engaging new media such as interactive webinars and podcasts. To discuss your policy and communication requirements, you can reach us on 020 8455 2126.
Best wishes for a healthy and happy 2019.