by Tanya HAFFNER | Jan 17, 2019 | Hot Topics in nutrition, The Nation’s Health
What’s hot in the wacky world of wellness in 2019
Historians believe that the practice of New Year resolutions originated in the Babylonian Kingdom, over 3,000 years ago. New Year intuitively brings time for pause, reflection and setting intentions for the year, and for many, that can centre on resetting what they eat, especially after indulging over the holidays.
In their annual round-up of the more bizarre fad diets for 2019, the BDA have suggested that the blood type diet, drinking your own pee (yes, really), detox teas/skinny coffee, slimming sachets and alkaline water, are some of the more bizarre regimes they’re coming up against.
Here’s a look at what else is hot in the wellness space, with some links to relevant, recent research that may help you in your daily communications or practice.
Lasting fasting
One thing that has remained popular as we come into the New Year, has been the idea of fasting and this month, Jurassic World actor Chris Pratt, announced to his 22.2 million followers that he’s doing the Daniel Fast.
If you haven’t heard of it, the Daniel Fast was created over a decade ago by Susan Gregory, according to the website, a ‘lay minister, businesswoman, coach for Christian living and wannabe techie’ and is a 21-day period of prayer and partial fasting practised by some Christians, based on the experience of the Prophet Daniel’s and Jewish fasting principles. According to the website, the permitted foods centre around vegan options, with some additional restrictions including all sweeteners (non-nutritive and nutritive), processed foods and solid fats.
Elsewhere and currently number 2 on Amazon.co.uk’s bestseller list for diet books, is Michael Mosley’s ‘The Fast 800’ (in fact it appears twice in the top-10 as a hardback and paperback). His latest offering since the popular 5:2 diet and 8-week Blood Sugar Diet (also still in the top-20), which centres on intermittent fasting/‘time-restricted eating’, is a low-carb, Mediterranean-style diet, based on only 800 calories.
For some recent papers on intermittent fasting in the past year, see the following links:
Flipping the Metabolic Switch: Understanding and Applying the Health Benefits of Fasting
Intermittent Fasting: Is the Wait Worth the Weight?
Compensatory Mechanisms Activated with Intermittent Energy Restriction: a Randomized Control Trial
Intermittent Fasting and Cardiovascular Disease: Current Evidence and Unresolved Questions
Veto keto
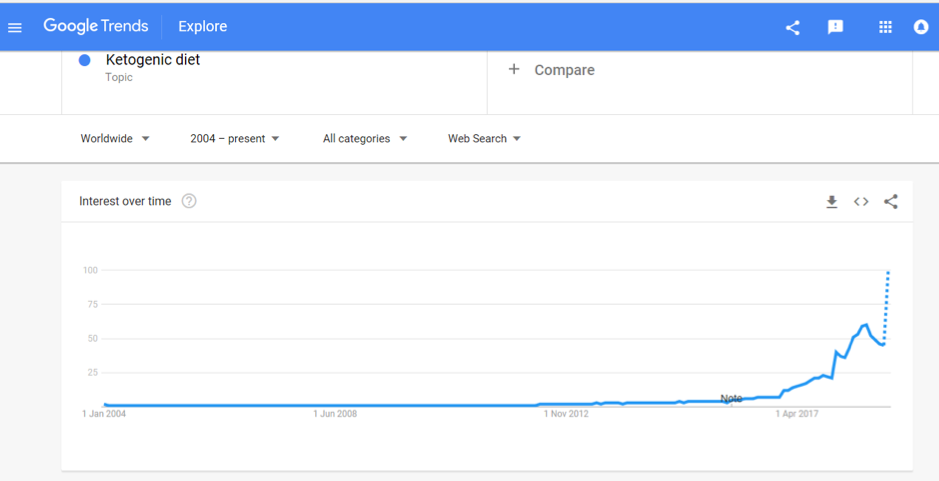
Also vying for the top spot of popular diets in 2019 is the Ketogenic Diet. A quick check of Google search trends shows that after bubbling away for the past few years, interest in this diet is starting to soar and it was the most searched diet term in 2018:

Being low-carb, high fat, the ‘traditional’ Keto Diet may jar against principles of plant-based eating, with new research in The Lancet reaffirming the importance of fibre (from vegetables and wholegrains) in the diet. Keto fans looking for a vegan or vegetarian version of the diet may instead opt for the plant-based version; dubbed ketotarianism, reminiscent of the pegan (paleo-vegan) that was also popular in 2018.
For some helpful papers on ketogenic diets published in the past year, see the following links:
A Nutritional Perspective of Ketogenic Diet in Cancer: A Narrative Review
A Systematic Review of the Use of Ketogenic Diets in Adult Patients with Cancer
The Ketogenic Diet in Disease and Development
Ketogenic Diet for Treatment of Intractable Epilepsy in Adults: A Meta-analysis of Observational Studies
Wellness woo
The Times has also just published an interesting article (which is unfortunately behind a paywall) which to sum up, provides (rather alarming) insight into what’s on the cards for ‘wellness revolutionaries’ in 2019; citing pink coconut water, quartz crystals, salt lamps, MCT oil, edible coffee bars and tongue-scraping, amongst other endeavours, all seemingly in the pursuit of health.
On the other hand, continuing to get good traction is the interest in digestive health and the microbiome, and plant-based eating, with Pinterest’s list of 100 emerging trends for 2019, reporting that searches for oat milk increased in popularity by 186% last year.
It is probably unfair to drop all these increasingly popular approaches into a fad bucket. Some, such as intermittent fasting, have a promising and growing evidence to their name and others may have snippets of beneficial principles in them, such as being plant-based, Mediterranean-style eating or with a focus on minimally processed foods.
Others, however, lack any credibly with regards to the claims they are making; often having inflated what is otherwise an incomplete evidence-base or simply just making things up.
In this era of ‘nutrition folk wisdom’, now more than ever is expertise needed from qualified dietitians and nutrition professionals to make sense of what is becoming an increasingly confusing dietary minefield.
Are there other trends that other dietitians or registered nutritionists do find helpful? Do let us know your thoughts. Or if you are a company and an organisation planning what trends you should support we are always happy to discuss and advise. Call us for a hello on 020 8455 2126 or email hello@nutrilicious.co.uk

by Tanya HAFFNER | Nov 20, 2018 | Hot Topics in nutrition
We were delighted that a record number of people joined us for last weeks’ Sustainable Diets NutriWebinar. The effect our food choices are having on the environment – and what we can do about it – is clearly a topic that matters to you.
Today, many months of in-depth work on sustainable diets comes to fruition with the launch of the British Dietetic Association’s (BDA’s) One Blue Dot campaign, aiming to ensure that dietary guidance is synonymous with health and sustainable eating.
Putting together the One Blue Dot programme
Throughout 2018, we’ve been part of a working group collating and reviewing the latest evidence from around the world on environmentally sustainable and healthy eating patterns, drilling down to macronutrient level.
Supported by project partner Alpro, the ground-breaking results have been brought together into the new One Blue Dot reference guide and toolkit. It’s aimed at dietitians, health professionals and influencers – and really everyone involved in food provision in some way.
Indispensable reference guide and resources
Launching today at Food Matters Live in London, we hope One Blue Dot will become an essential read, guide and inspiration.
Polls show that where 50% of us are likely to consider dietary changes to reduce the impact on climate change, in reality there are significant barriers to changing behaviour for the majority of people.
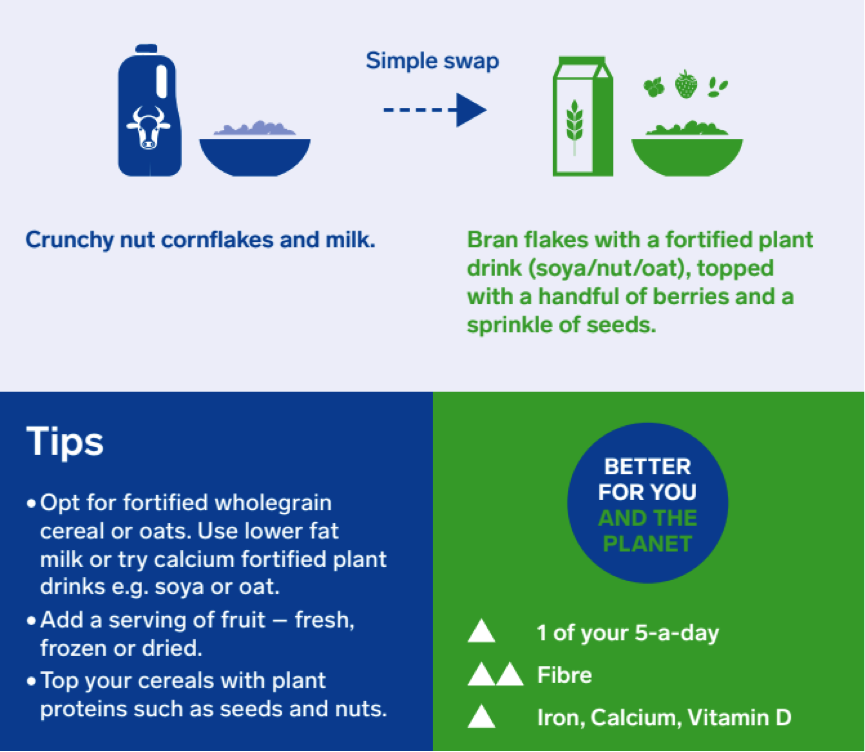
One Blue Dot aims to tackle this problem. It provides both the latest evidence and a bank of practical resources, including menu swap suggestions for breakfast, lunch and dinner:
A nine-point plan includes:
- Reductions in red and processed meat to 70g per person per day (also recommended by the World Cancer Research Fund).
- Prioritising plant proteins such as beans, nuts, soya and tofu.
- Consuming fish from sustainable sources.
- Moderating dairy consumption and using fortified alternatives where needed.
- Focussing on wholegrain starchy foods.
- Opting for seasonal, locally sources vegetables/fruit. Avoiding air freighted, pre-packed and prepared vegetables/fruit.
- Reducing overconsumption of high fat, sugar, salt foods.
- Making tap water and unsweetened tea / coffee the choice for healthy hydration.
- Reducing food waste, especially of perishable fruit and veg by choosing tinned/frozen alongside seasonal fresh produce.
Each is covered in depth, from the point of view of both the effect on the planet and nutrition.
Dietitians can help lead the way
As dietitian and working group member Ursula Arens brilliantly sums it up, “Eating healthy is for you; environmentally sustainable eating is for your children and their children.”
And – as the guide itself says – dietitians are ‘perfectly placed’ to communicate national and international guidance to help the public understand what they need to do to improve their own health and that of the plant to help future generation. The toolkit will be a ‘live’ document, with regular updates and extra information as the science develops.
We’d love to hear your thoughts about the topic and the guide!
Members can download the reference guide and tools at https://www.bda.uk.com/onebluedot
For press enquiries, call 0800 048 1714

by Tanya HAFFNER | Oct 8, 2018 | Hot Topics in nutrition, The Nation’s Health, Changing mindset
The most recent government guidelines on fibre intake recommend 30g per day for adults. Levels are currently at just 20g per day for adult men and 17.1g per day for women – that’s an average 68% increase in intake needed to meet recommendations.
And it’s not just adults: there’s a significant disparity between recommended and actual fibre intake across all age groups.
So why is fibre so important? And what can we do to help people meet the recommended intake levels?
Here’s a quick overview. To explore the topic in more detail, join our upcoming Fibre NutriWebinar, on Wednesday 7 November.
The benefits of fibre
Dietary fibre has long been recognised for its health benefits. But it’s only in recent years that our understanding and appreciation of it has significantly progressed.
Fibre’s health effects mainly result from two key factors – its physical properties (eg stool bulking, viscosity, binding ability) and its effect on the gut microbiota and luminal environment.
Amongst its many beneficial properties, clinical trials have proven that fibre:
- Decreases blood pressure
- Increases satiation
- Decreases glucose absorption
- Increases bacterial a faecal mass (commonly associated with health benefits including reduced risk of colon cancer)
- Exerts benefits through gut microbiota
Where are we getting our fibre from?
The main sources of fibre in the UK are cereals, vegetable and potatoes, contributing to 70% of total intake.
Interestingly, white bread and potato products prepared with fat (eg chips and crisps) are significant contributors. This is despite the fact that they have comparatively low fibre content, showing that consumption is high.
One of our challenges is to educate the public on healthier fibre sources – fruit, vegetables, whole grains and pulses, rather than broad recommendations on increasing cereals.
Understanding and helping consumers
We know that despite the convincing body of evidence for the role of dietary fibre in many chronic conditions, translating and achieving fibre recommendations in practice can be challenging.
Understanding the key barriers faced by the public and putting forward strategies to overcome these is key to facilitating better health for all.
Find out more about the FREE Fibre NutriWebinar with Dr Megan Rossi, RD and register now.
It’s one of our ongoing NutriWebinar series examining key nutrition topics with experts in the field.

by Tanya HAFFNER | Sep 12, 2018 | Hot Topics in nutrition, The Nation’s Health, Education, Changing mindset
The government recently announced new measures to halve rates of childhood obesity by 2030 and significantly reduce the health inequalities that persist – closing the gap in obesity rates between children from the most and least deprived areas.
This proposal builds upon the first chapter of the Childhood Obesity Plan, which was widely criticised at the time as lacking the breadth and depth of initiatives needed to effectively tackle such a widespread and entrenched issue.
Steve Brine, Public Health Minister has stated: “One in three children are now overweight or obese by the time they leave primary school. Overconsumption, combined with reduced activity, is having a catastrophic effect on our children’s health. As both a parent and minister, I am committed to driving today’s pledge of halving obesity over the next 12 years with bold new action.”
“Our updated plan will put parents in charge, providing more information and support. Our aim is to help families make healthier choices, which will in turn provide a better chance at a longer, healthier life for our children.”
Obesity – A systems issue
The financial burden of obesity is too great to ignore: it’s estimated that the NHS in England spent £6.1 billion on overweight and obesity-related ill-health in 2017/18, which, to put into context is more than was spent on the police, fire service and judicial system combined. The wider costs to society of these conditions are around £27 billion a year, if not higher.
Ever since the Foresight report was published over a decade ago, it has been recognised that obesity is a systems issue and one that therefore requires reform at many points, to deliver change. This idea and the fact that no plan to date has sought to address childhood obesity in a multi-sector way, was reiterated in the recent inquiry by the parliamentary Health and Social Care Committee into childhood obesity. Childhood Obesity: Time for Action argued for a change in narrative, making clear that obesity is everyone’s business and “an effective childhood obesity plan demands a holistic, joined-up, ‘whole systems’ approach with clear and effective leadership”.
How does the Childhood Obesity Strategy measure up?
This update to the Childhood Obesity Strategy is a welcome step forward. It contains a raft of proposed measures that seek to tackle the issue using a co-ordinated range of policy levers. What is also good to see is that this new plan takes a firm but fair approach in how it will deliver change: using voluntary measures in the first instance but being clear that a harder tact with the likes of regulatory and fiscal measures will be considered where progress is deemed insufficient, or where a level playing field is required.
Here at Nutrilicious, we’ve taken a closer look at what’s in store and benchmarked the new childhood obesity plan against the World Cancer Research Fund’s NOURISHING framework, as well as the recommendations from the Health and Social Care Committee’s report mentioned earlier.
The NOURISHING framework
The NOURISHING Framework sets out that policies are needed within three core areas to improve diets: the food environment, food system and behaviour change communication.
N – Nutrition label standards and regulations on the use of claims and implied claims on food
O – Offer healthy food and set standards in public institutions and other specific settings
U – Use economic tools to address food affordability and purchase incentives
R – Restrict food advertising and other forms of commercial promotion
I – Improve nutritional quality of the whole food supply
S – Set incentives and rules to create a healthy retail and food service environment
H – Harness food supply chain and actions across sectors to ensure coherence with health
I – Inform people about food and nutrition through public awareness
N – Nutrition advice and counselling in health care settings
G – Give nutrition education and skills
Bearing in mind that some policies and actions targeting childhood obesity were in place prior to this strategy update, overlaying the new measures show how broad their impact alone intends to be:
| New measures |
N |
O |
U |
R |
I |
S |
H |
I |
N |
G |
Nutrilicious notes |
| Improved food labelling to display ‘world-leading, simple nutritional information’ as well as information on origin and welfare standards following Brexit |
X |
|
|
|
|
|
|
|
|
|
|
| Strengthen School Food Standards to reduce sugar consumption |
|
X |
|
|
|
|
X |
|
|
|
We would like to see these universally applied and close the loophole that exists for some academies |
| Strengthen Government Buying Standards for Food and Catering Services* |
|
X |
|
|
|
|
X |
|
|
|
|
| Ban price promotions such as buy one get one free, multibuys or unlimited refills of unhealthy foods and drinks in the retail and out of home sector* |
|
|
|
|
|
X |
|
|
|
|
It is good to see a mandatory approach applied here, as this is what is undoubtedly needed when policies will impact businesses’ bottom line. |
| Ban the sale of energy drinks to children* |
|
|
|
|
|
X |
|
|
|
|
|
| Ban promotion of unhealthy food and drink by location e.g. positioning – checkouts, end of aisles and store entrances, in retail and out of home sector* |
|
|
|
|
|
X |
|
|
|
|
|
| Introduce a 9pm watershed on unhealthy food and drink advertising and similar protection online* |
|
|
|
X |
|
|
|
|
|
|
We would like to see similar controls applied to sports advertising |
| Review governance arrangements for advertising rules (currently overseen by the Committee of Advertising Practice and Advertising Standards Authority) |
|
|
|
X |
|
|
|
|
|
|
|
| Potentially bring ‘sugary milk drinks’ into the soft drinks levy if insufficient action on sugar reduction takes place |
|
|
X |
|
X |
|
|
|
|
|
|
| Introduce mandatory calorie labelling for out of home sector in England* |
X |
|
|
|
|
X |
|
|
|
|
|
| Sugar reduction plan for products aimed exclusively at babies and young children due in 2019* |
|
|
|
|
X |
|
|
|
|
|
|
| Calorie reduction plan due mid-2019* |
|
|
|
|
X |
|
|
|
|
|
|
| Develop trailblazer programme with local authority partners to highlight what can be done within existing powers |
|
|
|
|
|
X |
|
|
|
|
We would like to see greater powers for local authorities and health services |
| Develop plan to use Healthy Start vouchers to provide additional support to children from lower income families* |
|
|
X |
|
|
|
|
|
|
|
|
| Ofsted will review school curriculum to understand how it can better support healthy behaviours, including food choices |
|
|
|
|
|
|
X |
|
|
X |
We would like to see improved early years education for parents to support a healthy first 1000 days and compulsory home economics with healthy cooking skills at the core in both primary and secondary schools |
*Proposal for further consultation
Is it enough?
While we applaud this latest round of the childhood obesity plan, we would also draw attention to the fact that there is still some way to go.
By mapping the proposed policy options against the NOURISHING framework, we can see that in this latest iteration of the plan much more focus has been given to shaping an environment that enables and supports healthier choices, which is great to see.
However, what is noticeably absent is the ‘I’ in terms of improving food and health literacy of the population. In a ‘post truth’ world where consumers are increasingly sceptical of messages coming from the scientific community, and when social media influencers are capturing the hearts and minds of the masses with questionable dietary advice, never has it been more important to provide clear, simple and authoritative information and advice. As such, we’d like to the see the government step-up their efforts on social marketing and educational campaigns.
What is more, a number of recommendations made in the Health and Social Care Committee are notably absent, including:
- Establishing a Cabinet-level committee to review the implementation of the plan, ensuring it gets the high-level traction it requires
- Proposing further measures around early years and the first 1,000 days of life, including targets to improve rates of breastfeeding
- Banning the advertising and promotion of follow-on formula milk
- Providing local authorities with further powers to limit unhealthy food and drink advertising near schools (the only powers available to local authorities extend to the positioning of the billboards themselves, not the content of the advertising)
- Introducing services for children living with obesity
Finally, while this plan is overtly focussed on limiting unhealthy foods and drinks and making processed, packaged foods a little better through reformulation (lower in salt etc), we would also like to see equal attention given to measures that work improve the quantity and quality of foods that we do want people to eat more of. Changing the dietary landscape will require strong efforts to provide families with the tools and knowledge to instil these healthier behaviours in a sustainable way.
The full plan for action can be viewed here:
https://www.gov.uk/government/publications/childhood-obesity-a-plan-for-action

by Tanya HAFFNER | Aug 1, 2018 | Hot Topics in nutrition, The Nation’s Health, Surveys and insights
An extensive detailed analysis of the current scientific evidence into omega-3 seems to have thrown a spanner in the works for heart health dietary advice.
Conducted by Cochrane, the review concludes that there is no correlation between cardiovascular health and intakes of the long chain omega-3 fats eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) over a one- to six-year period.
Long chain omega-3 fats have long been associated with reductions in blood triglycerides, blood pressure and thrombosis; producing anti-inflammatory and anti-arrhythmia effects as well as improving endothelial function and insulin sensitivity.
This most recent publication will raise many eyebrows within the heart health professional arena and likely to be taken up by media editors who seem to enjoy questioning the trustworthiness of public health guidelines. These recommend a diet including omega-3, especially found in oil-rich fish such as salmon, tuna and mackerel.
So, do we need to change dietary guidelines on the importance of omega-3 and oil-rich fish?
Before we jump the gun, it’s important to put things into context:
1. The shortcomings of the review
a. The studies investigated in this review predominantly used omega-3 supplements. Thus the outcomes cannot be related to oil-rich fish consumption which is the main dietary source of EPA and DHA.
b. The studies were also of one to six years’ duration, which is a relatively short period to assess disease and mortality risk. And conclusions cannot be reached for a lifetime consumption of foods rich in EPA or DHA.
c. Many of the studies may not have used adequate number pf subjects in the studies to elicit a result. This is especially the case for studies conducted in healthy individuals (and therefore low risk of heart disease), which would require very high numbers to demonstrate a difference in the omega-3 and non-omega-3 study groups.
d. Any studies conducted over the last two decades of people at risk of cardiovascular disease (CVD) will be in individuals already medicated with statins and other cardio-protective drugs, which may mask the effect, if any, of additional omega-3.
2. Omega-3 benefits go beyond heart health
Long chain omega-3 fats are critical for eye and brain development of the foetus and young children. Therefore, food sources should be included in a healthy balanced diet of children and adults planning for a family.
3. Oil-rich fish is not just omega-3. It offers so many health benefits.
a. Unlike omega-3 supplements, oil-rich fish is a rich source of not only the long chain omega-3 fats but also of selenium, zinc, vitamin D and iodine; woefully lacking in the UK diet.
b. Oil-rich fish has a healthier fat profile when compared to red meat and other animal proteins. Replacing saturated fat with unsaturated fat in the diet has been proven to have a positive effect on blood lipids and cardiovascular health (as confirmed by Cochrane’s 2015 review and the SACN’s & the WHO’s draft 2018 reports). See our saturated fat blog
Indeed, the authors themselves remind us of the other nutritional benefits of oil-rich fish and that this review does not negate public health advice that consuming oil-rich fish is beneficial to health.
The Nutrilicious view
Taking vitamin and mineral supplements as a substitute for eating a healthy balanced diet has never been encouraged by health professionals. However, dietitians recognise that when demands for specific nutrients are high, or when an individual’s nutritional intake is at proven risk of being compromised, supplements can play an important role. For example, pregnancy and folic acid; under-5 year olds and vitamins C and D; or sufferers of osteoporosis and calcium and vitamin D.
Therefore, these findings do not come as any surprise: omega-3 supplements are not a solution to better heart health. There are numerous dietary and lifestyle factors that impact on heart health. It should always be about food rather than the benefits of single nutrients.
As Linda Main, Dietitian and dietary advisor for cholesterol charity HEART UK, explains: “We continue to advise the lifelong consumption of a heart healthy diet centred around eating whole foods rather than the emphasis being on nutrients.
“Eating patterns such as the Mediterranean, DASH or the UCLP© diets result in the consumption of a nutritionally appropriate diet. This is characterised by eating plenty of vegetables, fruits, wholegrains, vegetable proteins such as nuts and soya, seeds, vegetable oils and spreads. In those who consume animal proteins, the inclusion of low fat dairy, lean and largely unprocessed meat and white and oily fish and seafood are recommended.
“Omega-3 supplements are not currently advised by HEART UK and would not be our first choice, except when prescribed by a recognised qualified health professional or when needed to safeguard the intake of the essentially fatty acid – alpha-linolenic acid.”
As oil-rich fish is an excellent low saturated fat protein source, and the main dietary source of long-chain omega-3 fats as well as other crucial nutrients, it should continue to be part of dietary guidelines.
Additionally, for those wishing to follow a more plant-based diet, it’s reassuring that the report finds consumption of the shorter chain omega-3 fats found in plant foods (like rapeseed and soya oil) has cardio-protective qualities. This supports findings from population studies that vegetarians and vegans have a lower incidence of cardiovascular events and mortality compared to non-vegetarians.
Current UK heart health dietary advice remains unchanged:
- Lower the amount of food eaten which is high in saturated fat and replace it with foods high in unsaturated fats (which Cochrane’s 2015 review supports, SACN 2017 Saturated fat draft guidance).
- Increase our intake of fibre (especially from beans, pulses, oats and barley), nuts.
- Consume at least five servings of fruit and vegetables daily.
- Reduce intakes of red meat and avoid/limit processed meat.
- Consume two portions of fish weekly – one of which should be oil rich.
- Increase intakes of leaner and plant-sources of protein.
- Use sterol or stanol fortified products (if blood cholesterol is raised after other dietary changes have been made).
It’s interesting to note that, unlike the US, the UK does not (and has never) recommended taking dietary supplements of omega-3 fish oil.
For up to date expert advice on heart health visit: heartuk.org.uk
Further references
Saturated fat and heart health reports
Supplements for specific groups
NHS UK: Vitamins for children; Vitamins, supplements and nutrition in pregnancy
Vegetarian and vegan diets and health outcomes
- Rizzo N, Jaceldo-Siegl K, Sabate J et al. Nutrient profiles of vegetarian and non-vegetarian dietary patterns. J Acad Nutr Diet.. 2013;113(12):1610-9.
- Sobiecki J, Appleby P, Bradbury K et al. High compliance with dietary recommendations in a cohort of meat eaters, fish eaters, vegetarians, and vegans: results from the European Prospective Investigation into Cancer and Nutrition-Oxford study. Nutr Res.. 2016;36(5):464-77.
- Springmann M, Godfray H, Rayner M et al. Analysis and valuation of the health and climate change cobenefits of dietary change. Proc Natl Acad Sci U S A.. 2016;113(15):4146-51.
- Clarys P, Deliens T, Huybrechts I et al. Comparison of nutritional quality of the vegan, vegetarian, semi-vegetarian, pesco-vegetarian and omnivorous diet. Nutrients.. 2014;6(3):1318-32.
Cochrane is an established body of researchers, health professionals and patients across the globe renowned for their high quality scientific reviews of nutrition and health evidence.

by Tanya HAFFNER | May 25, 2018 | Hot Topics in nutrition, The Nation’s Health
This week, Public Health England (PHE) published their first assessment on the government’s sugar reduction programme, introduced to help reduce rates of childhood obesity.
The food industry – including retailers, manufacturers, restaurants, cafes and pub chains – was given the target to cut 20% of sugar from a range of products by 2020, with a 5% reduction in the first year. The first year of the programme was from August 2016 to August 2017.
What does the assessment show?
- Retailers and manufacturers have achieved only a 2% reduction in sugar.
- Sugar has been reduced by 11% by retailers and manufacturers in drinks that are included in the Soft Drinks Industry Levy and average calories per portion has been reduced by 6%.
- New guidelines have been published for the drinks industry to reduce sugar in juice and milk-based drinks.
Importantly, PHE highlight that there are forthcoming sugar reduction plans from the food industry and that some changes of products were not captured in the data (as the changes took effect after the one-year mark measured). This all points towards hopefully seeing greater reductions in future assessments.
Measuring the progress
Ten food categories were measured that contribute the most sugar to children’s diets, although breakfast pastries and cakes were not included due to insufficient data. Some of the key findings from the assessment include:
- Reductions in sugar levels were seen across five of the categories.
- Yogurts and fromage frais, breakfast cereals, and sweet spreads and sauces have all met or exceeded the initial 5% sugar reduction ambition.
- Biscuits and chocolate confectionary have seen no change at all in sugar levels.
- The puddings category has actually seen a slight (1%) increase in sugar content overall.
- It has been noted that for the eating out of home sector, portion sizes in products likely to be consumed in one go are substantially larger (on average more than double) those of retailers and manufacturers.
- Calories in products likely to be consumed in one go have reduced in four categories. Of these, ice cream, lollies and sorbets, and yogurts and fromage frais have reduced average calories by more than 5%. Often this is due to smaller portion size.
The British Retail Consortium (BRC) provided an interesting infographic showing how the food industry has been cutting sugar.

In response to the PHE assessment, Andrew Opie, Director of Food Policy at the BRC, stated: “Retailers are fully committed to helping improve the health of their customers and have led the way in reducing sugar in their products. Thousands of tonnes of sugar have been removed from retailers’ own product ranges to date and continuing work will result in even greater reductions over the next few years.
“Retailers have shown that reducing sugar levels across a wide range of products is possible but all food businesses must follow suit if we are to see significant reductions in the level of sugar in the nation’s diet.”
The British Dietetic Association‘s Head of External Affairs, Jo Instone, said: “We recognise that there are limitations in the data and that these are the early stages of the reformulation programme. However, it is disappointing to have such significant gaps and for a number of manufacturers to have refused to allow information on their progress to be published.”
“Clearly, it will be important for the BDA, the Obesity Health Alliance and others to continue working with Public Health England and the government to drive this programme forward. We would hope that the 2019 report can fill in a number of gaps and that we will see more substantial progress made across the board.”
Milk based drinks and juice
Following our concern about sugar levels in fruit juice, we’re pleased to see new plans by PHE encouraging the drinks industry to achieve the following by mid-2021:
- Reduce sugar in juice-based drinks by 5% (excluding single juice – that is, products with juice from a single fruit with nothing added to it).
- Cap all juice-based drinks (including blended juices, smoothies and single juices) likely to be consumed in one go to 150 calories.
- Reduce sugar in milk (and milk substitutes) based drinks by 20% and cap products likely to be consumed in one go to 300 calories.
What’s next?
Some progress has been made, but it seems we’re still well off hitting targets for sugar reduction. It’s clear that more work is needed – by manufacturers and retailers, but also cafes and restaurants, where calorie intake tends to be significantly higher.
The next progress report from PHE is due in Spring 2019 and should give a clearer picture on the programme’s progress.
Of course, this is only one of the many strategies needed to help combat the obesity crisis. Along with the BDA and many others, we’re looking forward to hearing government measures for issues including broadcast advertising, in-store promotions and other interventions to help tackle the problem.