by Nutrilicious | Jun 14, 2019 | The Nation’s Health
‘The levy is working.’ That’s the conclusion from a recent survey of drinks sales, a year on since the Soft Drinks Industry Levy (SDIL) – or sugar tax – was introduced.
The study concentrated on products that sell in large enough volume to have a public health effect. In a ‘historic change’, sales of Coke Zero Sugar increased by 50 per cent and Pepsi, sugar-free Max by 17 per cent. Full sugar Classic Coke and Blue Pepsi sales both fell.
The shift is attributed to the sugar free drinks being cheaper than their full sugar equivalent, as a result of the SDIL. Giving consumers the economic incentive to buy drinks that are healthier has worked. As the authors of the study say, ‘Discounts have had the effect that economists expected and health specialists hoped for.’
New sugar free versions of popular drinks are being increasingly sold in major retailers, with the hope that they’ll also become more prominent in smaller, independent shops. The positive trend is moving in the right direction – and it’s happening relatively quickly.
More needs to be done from a retail environment point of view, especially alerting customers to the discounts. Non-lead brands do still have work to do on reducing their sugar levels – although affecting a far smaller number of individuals, they still impact on health. And of course, the drinks industry is just one part of the wider obesity story.
We wondered what the effect of the sugar tax would be when it was introduced. So it’s fantastic to hear the dramatic change that’s already happened – and we’ll be monitoring the year ahead with interest.
The study was carried out by Jack Winkler, Emeritus Professor of Nutrition Policy, London Metropolitan University and Tam Fry, chair National Obesity Forum. Go to BeverageDaily.com to read the full results

by Nutrilicious | Jun 3, 2019 | Hot Topics in nutrition
According to headlines, iodine deficiency is the latest threat to our health in the UK. What’s more, the media says, poor iodine status is due to the rise of veganism and our increasing love for plant-based drinks as milk alternatives.
The headlines focused on the fact that dairy milk is our main source of dietary iodine, whilst plant-based drinks (with a few exceptions) do not contain iodine.
But is lack of iodine an issue? Could an increased consumption of plant-based drinks put people at risk of iodine deficiency?
It’s a complicated issue, but let’s look at the facts…
Is iodine important in the diet?
Yes. Iodine is essential. The body needs iodine to make thyroid hormones, which is fundamental for foetal and young children’s growth and brain development. Severe iodine deficiency in pregnant women can cause irreversible brain damage in their offspring. Population studies have also demonstrated a lower IQ score of around 13 points in severe iodine-deficient populations compared to iodine replete populations. The World Health Organisation (WHO) has stated that low iodine status is the single most preventable cause of brain damage in the world.
Adequate iodine status is especially critical for women of child-bearing age, during pregnancy and whilst breast feeding, to ensure optimal brain development in the foetus and young infant. Continued optimum intake in childhood and adolescence is fundamental as the brain continues to develop. It is important to note that folate, iron and long-chain omega-3 fats are also critical to brain development.
Severe iodine deficiency is rare in developed countries like the UK. However, there are significant numbers of women, especially of child-bearing age who are mild to moderately iodine deficient. A number of recent meta-analysis (including findings from UK population groups) indicate a high probability of compromised cognitive development in children whose mothers had mild to moderate iodine status during pregnancy. How significant these lower IQ scores are to cognitive ability in adulthood has yet to be established.
Measuring iodine status of a population
Median urinary iodine concentrations (UIC) are the best way to assess the iodine status of a population or large group. This is because the iodine content of foods is too variable to rely on dietary intakes as a measure of iodine status.
How the WHO classifies iodine deficiency.
| For a healthy population 6 years and older |
For pregnant and breast feeding women |
| Median UIC is below 100mg/L AND
If 20% or more of that population has a median UIC of less than 50mcg/L. |
Median UIC below 150mcg/L |
| Mild deficiency |
50-99 mcg/L |
| Moderate deficiency |
20-49 mcg/L |
| Severe deficiency |
<20 mcg/L |
Does the UK have an iodine deficiency problem?
According to the latest National Diet and Nutrition Survey (NDNS) using WHO criteria, from an overall population perspective we’re actually not doing badly, with all age groups and sexes showing adequate iodine status.
However, severe to moderate deficiency (UIC <50mcg/L) still afflicts a significant number of our population:
• Approximately 1 in 10 children aged 4-18 years
• 14% of adults 19-64 years
Unfortunately, the NDNS does not currently perform UIC measures in pregnant women or the under 3s, the most susceptible population groups to low iodine status.
Women of child-bearing age (16-49 years) are classified as iodine replete, with a median UIC of 102mcg/L.
However, almost 70% of them would be classified as mildly to moderately iodine deficient if they were to become pregnant – i.e. UIC levels below 150mcg/L – when taking account for the increased demands of the foetus and young infant.
As a result, many are calling for the government to review the UK’s iodine initiatives, especially for women who are planning/are pregnant, or are breast feeding.
How does what we eat impact on our iodine levels?
The ocean is nature’s source of iodine, thus fish, seaweed and algae are rich sources. Additionally, coastal soil regions will acquire some iodine from coastal waters.
Therefore, higher intakes of seafood are paramount for adequate iodine status and studies have found seafood intakes to be positively correlated with iodine status.
In the UK, fish intakes are exceptionally poor. Few meet the government’s recommendation of two 140g servings per week. Average total fish weekly intakes in the UK:
• The majority of 4-18 year olds consume no more than 56g.
• The majority of adult women (19-64 years) consume 84g fish.
• The majority of adult men (19-64 years) consumer nearly 100g fish.
Iodine and dairy milk
In the UK, farming practices were changed in the 1930s to eradicate the high incidence of iodine deficiency. Animal feeds were fortified with iodine and the use of sterilizers containing iodine were introduced. This resulted in a significant increase in iodine levels of dairy milk and a consequent eradication of severe iodine deficiency.
Winter milk is significantly higher in iodine compared to summer milk, as dairy cattle are more likely to reared indoors with fortified feed in the winter months.
Thus the key source of iodine in the UK is indeed dairy milk – contributing to 34-40% iodine intakes in adults and 40-51% iodine intakes in 4-18 year olds.
Could plant-based drinks place the nation at risk of Iodine deficiency?
It is true that the majority of plant-based drinks do not contain iodine. However:
1. Incidence of mild to moderate iodine deficiency in pregnant women has actually been high in the UK since the 1990s, when milk intake was at its highest.
2. Despite the recent popularity of plant-based drinks, dairy milk intakes have seen little reduction. And plant-based drinks consumers also continue to drink dairy.
Since 2010, milk intakes have reduced by just 74mls per person per day (a 6.5% decrease), while plant-based drinks – although on a sharp incline – equate to just 45ml per person per day.
Therefore, plant-based drinks – whether they are or not fortified with iodine – are not the cause of the iodine deficiency that has been present for many decades.
Other considerations
• Cognition is affected by multiple environmental, psychological as well as dietary components e.g. pollutants, home environment, education level, various nutrients including vitamin D, iron, folate and iodine.
• Iodine is not highlighted in advice provided to expectant mothers, nor is it on the government agenda.
• No studies have indicated vegan populations, who exclude all dairy, to have lower IQ levels compared to omnivores.
There are also effective initiatives that have helped to eradicate severe iodine deficiency
• The WHO Iodized Salt programme has been adopted in many countries and proven to be successful.
• Iodine supplements have shown to be effective when given to women in the first or second trimester of pregnancy.
Takeaway messages
1. Many factors are at play when considering brain development of the foetus and young infant:
– Adequate intake of a number of nutrients, including iodine but also iron and folate
– Optimal environmental and psychological settings.
‘Fixing’ one aspect or one nutrient is not the answer to helping optimise cognition in the UK.
Saying this, iodine is one of the essential nutrients for brain development. That has been overlooked and needs to be addressed by the government, on a similar level to iron, folate and vitamin D – especially for expectant women and breast-feeding mothers. Monitoring iodine status needs to be instigated by the government for these groups and young children.
2. The increase in plant-based drinks’ popularity is not the cause of the sub-optimal iodine status in the UK, which has been prevalent in pregnant women for decades – way before plant-based drinks became mainstream.
Rather, the poor dietary patterns of the UK population need to be addressed, especially with regard to our less than optimal fish intake – the richest source of iodine.
Whenever we see the media headlines expounding the ‘benefits’ or ‘dangers’ of individual nutrients or foods, we worry. After 20 plus years in public health nutrition and communications, we believe there is a responsibility and an urgent need for all involved in this field to move away from doing this. In the majority of cases it’s not helpful and is more often scaremongering.
a. We need communications to focus on a balanced food intake. Focusing on a single nutrients in the media is dangerous and ignores all the bigger questions that need addressing: especially obesity and its many associated diseases and “how to” best help the nation enjoy a healthy balanced food intake for optimum health.
b. We need food and health communications that are not only healthy but also sustainable for our planet. Current scientific evidence repeatedly highlights the impact that our food choices have on the environment because of their significant contribution to greenhouse gas emissions, deforestation, biodiversity loss, and destruction of the ecosystem, use of fresh water and polluting of soil.
Beef and dairy cattle farming have been highlighted as the major dietary contributors, whereas plant-based drinks have been shown to be significantly more sustainable.
Leading experts have concurred that a balanced diet that is based predominantly on plant foods – including plant-based drinks – with lower intakes of meat and dairy, without having to exclude them altogether, is both sustainable and nutritious. Read our Sustainable Diets blog for more information.
It is incumbent upon all food and health influencers to incorporate these messages into all relevant food and health communications. Unfortunately, this is not yet being considered widely.
Sources:
1. Chambers L. Are plant-based milk alternatives putting people at risk of low iodine intake? Nutr Bulletin 2018;43:46-52
2. PHE. Results of the National Diet and Nutrition Survey (NDNS) rolling programme for 2014 to 2015 and 2015 to 2016. 2018 [cited 5/11/2018]
3. WHO-UNICEF. Assessment of iodine deficiency disorders and monitoring their elimination. Third Edition. 2008 [cited 9/25/2018]
4. Bath S, Rayman M. A review of the iodine status of UK pregnant women and its implications for the offspring. Environ Geochem Health 2015;37(4):619-29.
5. Levie D, Korevaar TIM, Bath SC et al. Association of maternal iodine status with child IQ: a meta-analysis of individual-participant data. J Clin Endocrinol Metab. 2019 Mar 28. [Epub ahead of print]
6. Dineva M, Rayman MP, Levie D et al. Similarities and differences of dietary and other determinants of iodine status in pregnant women from three European birth cohorts. Eur J Nutr. 2019 Feb 8. [Epub ahead of print]

by Nutrilicious | Apr 16, 2019 | The Nation’s Health, Changing mindset, Impactful health initiatives
We’re excited to be involved in a new initiative to help tackle the critical problem of poor diet amongst lower income households: Shop Well – Eat Well. It’s a collaboration between the British Dietetic Association (BDA), Alpro and the Southwark Hub, with the aim of a multi-angled approach to have a real and lasting impact.
Launched last month, we brought together experts to give their insights into key topics. Here’s a summary of some of the key points, followed by links to each of the presentations, which we highly recommend you take the time to watch!
People on lower incomes have a worse diet and shorter life expectancy
There is a direct correlation between diet and income, in turn affecting health. The lower your income, the more likely it is you will:
- Eat more sugar, processed foods, fat and sodium
- Eat less fibre, vitamin A and folate
- Be less likely to meet iron, folate and calcium recommendations
- Eat less oil-rich fish
- Eat more take-aways
- Cook less at home from scratch
People in lower income groups in the UK have a significantly shorter life expectancy than the average: by nine years for women and seven for men.
They have double the rates of cardiovascular disease, lifestyle-related cancers, type 2 diabetes and total mortality compared to the national average. Obesity prevalence of the most deprived 10% of children is approximately twice that of the least deprived 10%.
This is not new news. Countless attempts have been made to try to address the problem and encourage people on lower incomes to eat more healthily, thereby increasing their quality of life and life expectancy.
But when it comes to eating habits, behaviour change is very difficult to achieve.
Barriers to healthy eating are multiple, complex and interlinked – psychological, financial, environmental, conscious and unconscious. Among lower income households they include:
- Financial barriers – For low income families, a big barrier to buying new foods or going to a new food shop is not knowing how much the food will cost, or assuming that it will all be expensive. Parents want to know exactly how much their shopping basket is before they reach the checkout.
- Social barriers – Food habits get passed down the generations as young people grow up and become parents themselves. What children see their parents and families doing is what they grow up thinking of as ‘normal’.
- Preparation space – Cooking from scratch relies on kitchen equipment, confidence in cooking skills, time to prepare food and pleasant surroundings – not the case for many on low income.
- Limited bandwidth – The cognitive burden of living under financial strain and other modern day life stresses reduce parents‘ mental bandwidth; brainpower that would otherwise go to planning ahead and problem-solving.[1] Families in this situation look for quick and easy ways to eat, and takeaway and convenience foods provide an in-the-moment solution to feeding children quickly, affordably and safely.
- Advertising and shop layouts – Cues such as special offers, advertising for takeaways, attractive packaging and child-height shelving nudge families towards less healthy foods in shops.
- It’s not always a lack of knowledge or cost that’s a problem, it’s translating knowledge to practice.
In fact, most eating behaviour is driven by unconscious, habitual processes. These are largely immune to education when it comes to behaviour change. Yet this has been our predominant approach to changing dietary behaviour!
Breaking the habits of a lifetime
Multiple collaborative strategies are needed to succeed in changing behaviour: from government, local authority, industry and all food providers, alongside continuing to help individuals overcome their personal barriers.
We need to making healthy eating
- easy,
- habitual, and
- normal
As behavioural psychologist Dr. Paul Chadwick says, it’s not sustainable for people to have to think about every food choice that they make. Healthy eating has to become the default option.
A new initiative for change
Behavioural science shows the importance of interactions between the individual and their physical and social environment when it comes to habit forming and breaking.
It’s time the food environment changed to make healthy eating as easy to attain as possible for all, including low affluent groups.
It’s also time for families and individuals to be supported in overcoming barriers to breaking the unhealthy habits.
 We’re excited to be part of the new initiative, Shop Well – Eat Well, to help enable this – especially targeting those on a low income.
We’re excited to be part of the new initiative, Shop Well – Eat Well, to help enable this – especially targeting those on a low income.
Starting as a year-long pilot in Southwark, South London, it’s kicking off in June. Community charities and volunteers will join to create peer and professional-led healthy eating seminars and workshops tailored to the young, old and families.
At the launch, Kate Arthur, UK External Scientific Affairs & Nutrition Manager at Alpro, explained: “We wanted to find interventions that would encourage people to think about their food choices differently.
“Going directly into the community to find out what will work for people is the logical thing to do. We’ll be working on different engaging activities such peer led cookery workshops and drop in seminars, with help from the BDA Let’s get Cooking and an advisory committee of experts, always with an eye on the main barriers.
“Ultimately, we’ll be assessing to see what really makes a difference over the next year of the campaign and we’ll share any success stories widely with local communities nationwide and the dietetic community as a whole.”
Caroline Bovey, Chair of the British Dietetic Association added: “By partnering on this project, and working with the food manufacturers and shops that people are accessing daily, we’re excited to directly tackle some of the wider barriers to healthy habits in a local area. The BDA is delighted to be working with Alpro and the Southwark wellbeing hub to help people who often have to prioritise the other demands of daily life over their food choices.”
Take advantage of insightful presentations and useful resources
At our launch, five leading experts presented the latest evidence and initiatives to help overcome barriers to healthy shopping baskets and healthy eating. The presentations are available on the Shop Well – Eat Well website. Make yourself a cup of tea, watch, learn and be inspired:
– Dr Paul Chadwick, behaviour change leading expert: A scientific approach to behaviour change
– Sue Baic, Registered Dietitian: Affordable, healthy and sustainable eating in practice
– Duncan Brown, Development Director at charity Shift design: How does affluence impact on food choices?
– Kate Arthur, Alpro UK’s External Scientific Affairs & Nutrition Manager: Changing behaviour in the community
– Nilani Sritharan, Company Nutritionist at Sainsbury’s Supermarkets Ltd: Making healthy shopping easier
You’ll also find practical and engaging resources to help consumers overcome their barriers to healthy eating.
#shopwelleatwell @SouthwarkHub @BDA_Dietitians @Alpro

by Nutrilicious | Apr 25, 2016 | Food category comment
The growing trend for breakfasting on-the-go and at out of home establishments has been threatening breakfast cereal’s number one spot1. As well as a need for more convenience, breakfast cereals have been hit hard by the recent negative headlines with regard to their sugar content. But are the latest trends going to help improve or will they fuel the obesity epidemic?
What do the Brits fancy for breakfast?
Many surveys claim that up to 42% of us (and almost a quarter of school children) do not always have breakfast, stating time constraints are a major factor2,3. Kantar’s data however shows that only 7.7% of breakfast occasions were actually missed last year. This significant difference could be explained by the growing trend of eating ‘on-the-go’ or away from home which has grown by 10%4.
The UK seems to be slow to change its breakfast habits with the majority of breakfast occasions (84%) still taking place at home and breakfast cereals, toast and porridge remaining top favourites during the week whilst cooked breakfast continues to be popular at weekends2. The growing trend is for eating at catering establishments and portable on-the-go offerings with perceived health credentials such as breakfast biscuits, porridge pots and fruit and nut category, the latter seeing a 21.5% increase in 20152.
Breakfast cereals: UK’s no.1 choice with wholegrain cereals chosen by 37% of us during the week and still claiming over half the share of the market5,6. Many breakfast cereals have now significantly reduced their sugar levels, more ‘no-added-sugar’ variants are gaining shelf-space whilst a few indulgent variants still remain. According the to the latest National Diet and Nutrition Survey (NDNS), breakfast cereals account for just 5% of the added sugar intakes of adults and 6-8% of 4-10 year olds and teens.7 On the other hand, breakfast cereals (especially those that are fortified) do make a significant contribution to key vitamin and mineral intakes:
- B vitamins, in particular B1, B6 and folate.
6-9% of our vitamin D intake – vitamin D status is a growing concern in the UK6.
- Iron: 46% of teenage girls, and almost a quarter of women consume below the low reference nutrient intake (LRNI), which places them at high risk of deficiency. Cereals are a major source of iron contributing to 17% of teens, 23% of 4-10 year olds and 12% of adult intakes.
- Calcium: mainly due to the addition of milk but a handful are also fortified. Almost a fifth of teenage girls do not meet their LRNI placing them at higher osteoporosis risk in later life.
Looks like a hard act to follow, so how do other breakfast choices match up?
Porridge: Oats are making a come-back with 27% of us likely to make this choice in a week5. Porridge oats get a nutritional gold star from us, as they provide the gel-like fibre, beta-glucan, which has been proven to lower cholesterol levels – and boy almost 60% of us need to lower our cholesterol.8,9 However, how we serve them up is critical – piling on the sugar (even demerara sugar), drizzling with honey or syrup and making it with full cream milk converts this saint to a sinner. The porridge revival could be partly explained by the growing ‘on-the-go’ varieties which are now purchased by 9% of consumers4.
Toast continues to be popular for 32% of people during the week5. White toast provides calcium (accounting for 13% of teenagers’ intakes) whilst wholemeal and seeded breads provide fibre which, is highly relevant considering the 2015 new increased UK fibre recommendations6,10. Clearly, what we add to our toast is central to the nutritional quality, nut butters and unsaturated fat spreads providing healthy heart fats, whilst chocolate spreads (yes…that includes the favourite hazelnut and chocolate spread) and preserves are taking us on a sugar high.
Eggs: we can’t seem to get enough of them. Almost 3,000 million eggs are eaten at breakfast every year with one in five of us opting for an eggy breakfast at least once a week11. Eggs, originally classified as a complete nutrient food, provide protein, vitamin D, iron, phosphorus, iodine and selenium. In addition, it is reassuring to know that all the UK heart and health advisory bodies do not limit egg consumption (as the cholesterol found in food does not have a significant effect on blood cholesterol in most people)12. A gold star from us, if boiled or poached, however, the Brits favourite is a fried egg… oops, too much fat.
The growing convenience breakfast trends
Convenience, portability and time-saving options which also provide exceptional nutrition credentials are now in demand. A third of us are eating breakfast away of home at least once a week and 15% of us do so every day according to a Beacon 2015 survey13. In addition, gluten-free and high-protein health claims are also gaining traction4.
Out of home establishments:
- Greggs and MacDonald’s have a booming breakfast trade, however, the majority of options seem to include sausages and / or cheese which is a recipe for a heart attack with the hefty dose of saturated fat and salt levels. Some of the breakfast options providing up to 80% of daily saturated fat and over ¾ of daily salt recommendations. On the positive note, porridge oats are making an entry, however, for consumers to pick out the handful of healthier options amongst the sea of unhealthy options will be difficult. We feel a better balance and better promotion of healthier options are needed.
- Coffee shops: Coffees and other drinks on offer can be high in saturated fat and sugar laden, however, the options are there to opt for lower fat milks and sugar-free syrups. The mainstream coffee shops have improved their ‘healthier’ breakfast options with porridge, fruit salads, fruit and nuts and yogurt with granola on offer. However, the low fibre, higher fat and calorie croissants and muffins continue to be more popular.
- Cooked breakfasts: This is still a popular weekend choice, but with a whopping 800-1,000 calories for a classic fry-up, it has to have a thumbs down from us. Or does it? Making a few requests when ordering can bring this fat and calorie laden classic into healthy repute: poached eggs, beans, grilled lean bacon rasher, mushrooms, tomatoes, one sausage and toast instead of fried bread could almost half the calories whilst still providing fibre, protein as well as essential vitamins and minerals.
On-the-go options
Breakfast drinks, breakfast biscuits and fruit and nut bars have become widely available, albeit at a higher unit cost. All are portion controlled, the breakfast drinks use skimmed milk as the main ingredient and most provide a range of vitamins and minerals – many matching the nutrition profile of breakfast cereals.
Breakfast biscuits: 19% of consumers are opting for breakfast biscuits over cereal bars4. Nutritionally, they mimic cereals from macro and most micronutrients. Calcium and protein levels from the milk added to cereal are clearly lacking in the biscuits, but the leading brand provides clear advice on paring up the biscuits with yogurt and / or fresh fruit / fruit juice. An excellent option in our point of view.
Breakfast drinks: Definitely a very small but growing market that has failed to take off in the past. The Australian number one brand is definitely leading on this category. Many utilise key health slogans such as protein, energy and fibre whilst omitting to highlight their less than impressively sugar content. Nutritionally, they seem to match up with for fat and protein, however, sugar content varies between 18g and 20g per serving compared to cereal at 0-11g per serving. Interestingly, protein content can be exceptionally high and calcium levels per serving are 2 – 3½ fold greater than for most cereals served with milk. This may be advantageous if it appeals to the 19% of teenage girls and 12% of young women who have calcium intakes below the low reference nutrient intakes. Nutrilicious opinion: get that sugar down.
New opportunities
Recent government advice has highlighted the need to cut sugar levels (free sugars to less than 5% total energy intake) and increase fibre intake (to 30g AOAC per day for teens and adults)10. Considering this advice it would seem beneficial for any new breakfast foods to be based on wholegrains and / or provide soluble fibres such as beta-glucans and inulin and to be limited in free sugars as much as possible. The vitamin and mineral fortification of breakfast cereals significantly contributes to the nation’s micronutrient status, thus any new options must ensure that these essential nutrients are not lacking<sup>6</sup>. With on-the-go eating and eating at out of home establishments becoming more popular, it is paramount that options lower in sugar dominate. Sugar is now the big enemy under scrutiny by government, health organisations and pressure groups such as Action on Sugar14. This also applies to porridge pots and cereal pots as not all are low sugar and/or high in fibre. To add to the challenges for innovation, the consumer continuous to demand a great taste as well as a healthy nutrition quality.
Conclusion
When comparing different options, it is clear that healthier options are available whether breakfasting at home, catering establishment, coffee shop or eating on the go. However, the new trends need to focus more on providing a better balance and promoting more of the healthier options. The porridge, fruit and nut, lower fat and sugar free options at catering establishments are a good start, but the likelihood of the consumer choosing these amongst the overwhelming selection of higher fat, salt and sugar options is questionable. Breakfast cereals do contribute significantly to vitamin and mineral intakes especially iron and calcium – and there is a risk for vulnerable groups to become deficient if they begin to move away from these.
With all the above in mind, there are many opportunities to develop new innovative ways to create tasty, convenient, nutritious breakfasts that allow for people on the go to eat a greater variety of foods to help meet their nutritional requirements. Whilst time may be limited for many in the morning, Variety is King in helping consumers achieve adequate nutrient intake.
References
- Financial Times Oct 3 (2014). Daneshkhu S: Cereal sales go soggy as breakfast shrinks. http://www.ft.com/cms/s/0/771a89b2-4af2-11e4-839a-00144feab7de.html#axzz3zVYhDqes
- Agriculture and Horticulture Development Board (AHDB) for Cereals & Oilseeds Market News: Cereals and bread still breakfast mainstays. 14 January 2016. http://cereals.ahdb.org.uk/markets/market-news/2016/january/14/prospects-cereals-and-bread-still-breakfast-mainstays.aspx
- British Nutrition Foundation. National Pupil and Teacher Survey 2015 UK Survey Results. https://www.nutrition.org.uk/attachments/article/846/UK%20Pupil%20and%20Teacher%20Survey%20Results%202015.pdf
- Grocer March Guide to Breakfast.
- Shake Up Your Wake Up, Fun Breakfast Facts (2015). http://www.shakeupyourwakeup.com/why-is-breakfast-important/our-breakfast-foods/fun-breakfast-facts
- Bates B et al (2014). National Diet and Nutrition Survey: results from Years 1 to 4 (combined) of the rolling programme for 2008 and 2009 to 2011 and 2012. Available at https://www.gov.uk/government/statistics/national-diet-and-nutrition-survey-results-from-years-1-to-4-combined-of-the-rolling-programme-for-2008-and-2009-to-2011-and-2012
- Scientific Advisory Committee on Nutrition 2015. Draft Vitamin D and Health report. Scientific consultation: 22 July to 23 September 2015. Available at https://www.gov.uk/government/consultations/consultation-on-draft-sacn-vitamin-d-and-health-report
- Heart UK (2016). The Power of Oat Beta Glucan. http://heartuk.org.uk/images/uploads/healthylivingpdfs/HUK_factsheet_F09_OatBetaGlucanF.pdf
- Townsend N, Bhatnagar P, Wilkins E, Wickramasinghe K, Rayner M (2015). Cardiovascular disease statistics, 2015. British Heart Foundation: London. Available at https://www.bhf.org.uk/publications/statistics/cvd-stats-2015
- Scientific Advisory Committee on Nutrition (2015). Carbohydrates and Health Report. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/445503/SACN_Carbohydrates_and_Health.pdf
- Egg Info (2016). Industry Data. https://www.egginfo.co.uk/egg-facts-and-figures/industry-information/data
- Gray J and Griffin B (2009). Eggs and dietary cholesterol – dispelling the myth. Nutr Bull 36,199-211
- Beacon. Brits’ breakfast habits a big boost for the economy as people spend £76 million every day on eating out for breakfast. Survey 2015. Available at http://www.digitalnewsroom.co.uk/beacon/brits-breakfast-habits-a-big-boost-for-the-economy/
- Action on Sugar (2015). Breakfast Cereals Survey 2015. http://www.actiononsalt.org.uk/actiononsugar/Press%20Release%20/146900.pdf

by Nutrilicious | Mar 21, 2016 | Hot Topics in nutrition
Wednesday 15th March saw the nation’s health top of the government agenda with the launch of the new Eatwell Guide and more surprising, the new budget announcement declaring a tax for sweetened beverages.
We are still in the dark about the how much tax will be added, but it is thought that it will be set at the PHE recommendation of 20%, despite the National Obesity Forum recommendation to set it at 50% if any impact on behaviour change is to occur.
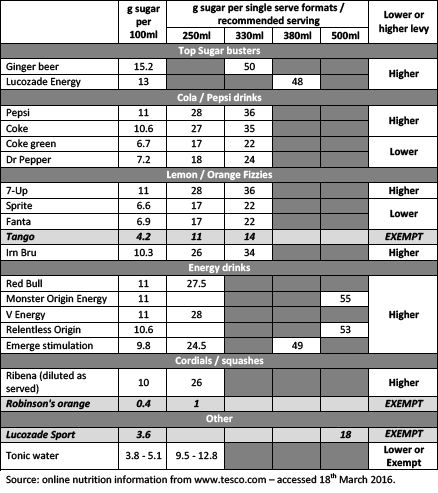
Which soft drinks will be hit?
Two tax levels will be set. One for soft drinks providing more than 5g sugar per 100ml and a higher levy for those providing more than 8g sugar per 100ml. The table below indicates how the current soft drinks market will be taxed.
Nutrilicious feels that single serve formats should have been taken into consideration when setting the sugar benchmarks, similarly to front of pack traffic light labelling. As an example, sports drinks are only available as a single 500ml serve bottle providing a total of 18g sugars, yet because they contain less than 5g sugar per 100ml, they will be exempt. This could be argued by other soft drinks companies as unfair. Many that will be taxed for containing over 5g or 8g sugar per 100ml, offer much small single serve formats, limiting the total serve sugar intake to the same as sports drinks and sometimes less.
Exemptions: fruit juice, milk drinks and small producers. This does muddy the waters somewhat as the government in its new sugars recommendations classified fruit juice as a ‘free sugars’ source and why are small producers exempt if they do produce high sugar drinks? Not quite an even playing field and this will not encourage innovation for lower sugar products from companies who will be exempt. Also, what does ‘milk drinks’ refer to? Will sugar laden flavoured milk drinks be exempt?
When will it be enforced? The tax will come into force in April 2018, giving manufacturers adequate time to reformulate their drinks and / or change their offerings to consumers. Many could try to reduce their sugars from the higher to the lower levy benchmark.
Will this reduce consumer purchase of higher sugar soft drinks? Possibly not, but the government is banking on this levy to add over £500 million to the economy which will be used to:
- Double the primary school PE and sport premium.
- Give 25% of secondary schools increased opportunity to extend their school day to offer a wider range of activities for pupils, including more sport.
- Expand breakfast clubs in up to 1,600 schools.
So, Jamie has won the battle to place taxes on sweetened drinks and this will be welcomed by health organisations even though many of them wanted to see a significantly higher levy. We do feel that a more even playing field should have been set and all high sugar drinks, including fruit juice and drinks from small producers, should have the levy enforced. In addition, single serve formats should be considered when assessing sugar levels. If anything, this could go a long way to help prevent consumers’ from being misled by marketing claims that a soft drink ‘is full of / provides energy’. A clever abuse by some manufacturers regarding consumer’s misunderstanding of the word ‘energy’ relating to healthiness rather than empty unnecessary calories. We look forward to more specific details.
A selection of current soft drinks on the market, their sugar content per 100ml and their single serve format or recommended serving size and which tax level they will incur in April 2018.

Sugar Drinks details
For further information on the 2016 budget: www.gov.uk/government/publications/budget-2016-documents/budget-2016